News • AML targetable immune escape mechanism
How leukemia cells trick the immune system
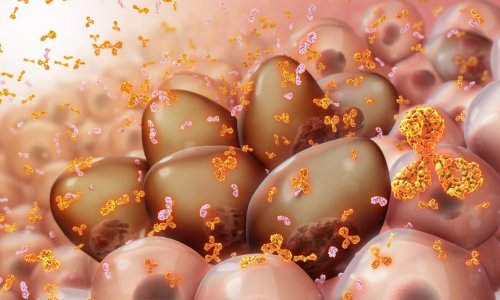
A research team at Lund University in Sweden has discovered a mechanism that helps acute myeloid leukemia cells to evade the body’s immune system. By developing an antibody that blocks the mechanism, the researchers could restore the immune system’s ability to kill the cancer cells in laboratory trials and in mice.
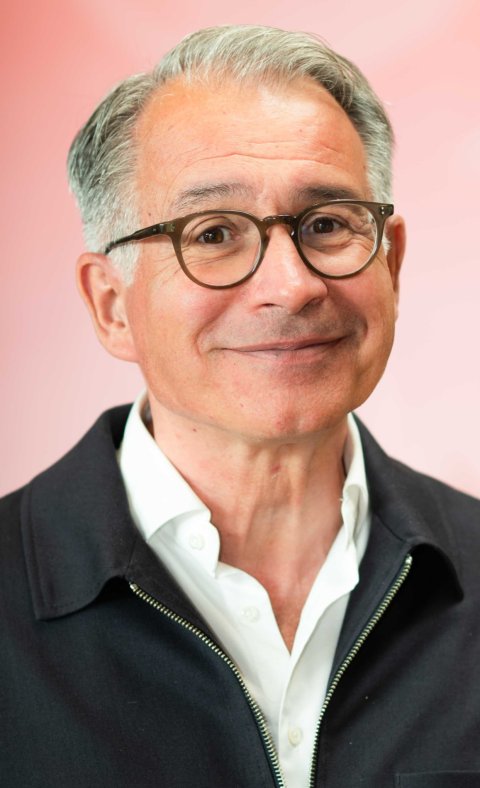
Image source: Lund University; photo: Tove Smeds
The discovery is published in Nature Cancer.
Immunotherapy has improved the treatment for many cancers, but progress has been limited in leukemia. Acute myeloid leukemia (AML) is particularly intractable, with a five-year survival rate of just over 30%. The existing treatments are often aggressive and may include both strong chemotherapy and stem cell transplantations.
“We wanted to see if we could find surface proteins unique to leukemia stem cells, and which would therefore act as interesting targets for a targeted treatment. If such proteins were not present on healthy blood stem cells it might be possible to attack the tumour – without harming the healthy blood system,” says Thoas Fioretos, research group leader and professor of clinical genetics at Lund University, and senior consultant at Skåne University Hospital.
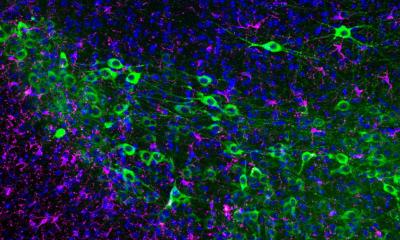
In the new study, the researchers identified a previously unknown surface protein that is expressed on the leukemia stem cells, but not on healthy blood stem cells. The discovery was enabled by a large-scale mapping of proteins in leukemia stem cells in bone marrow samples from three patients with particularly intractable AML. The mapping was then compared with the blood stem cells of healthy individuals. It was then that the researchers discovered the surface protein, SLAMF6, was only expressed on the diseased cells. The finding was then validated in an additional 50 AML patients.

Image source: Lund University; photo: Tove Smeds
The researchers then studied the protein’s function in CRISPR/Cas9 gene scissors experiments. The protein was shown to play a central role in how the cancer cells evade detection by the immune system’s T cells, which means that the cancer cells can continue to grow undisturbed.
It was also shown that the mechanism can be attacked. “When we blocked the surface protein, using a specific antibody we developed in cooperation with the SciLifeLab Drug Discovery and Development Platform, the T cells could suddenly detect and kill the cancer cells – both in test tubes and in mice,” says Carl Sandén, researcher at Lund University. He and Thoas Fioretos are the corresponding authors of the study.
It was like turning on the switch to the immune system again. When the surface protein does its job, it helps the cancer cell to elude the immune system, but by turning it off with the developed antibody, the immune system’s T cells could attack and kill the cancer cells.
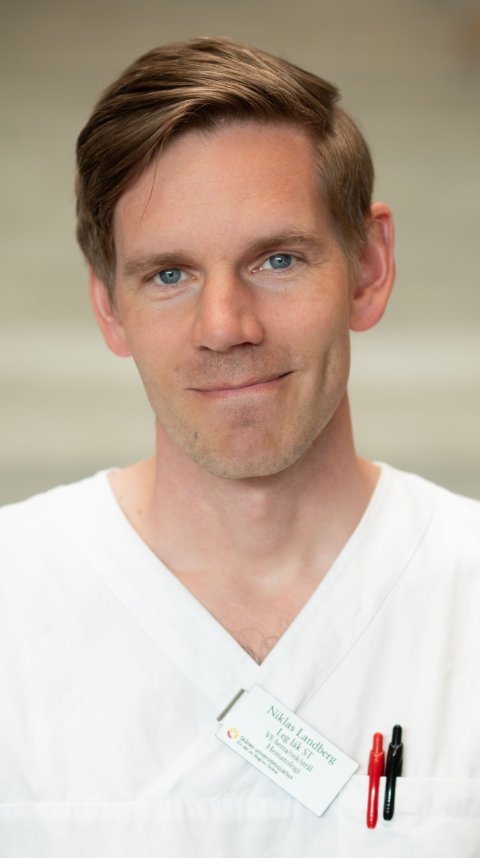
Image source: Lund University; photo: Tove Smeds
“Our discovery can partially explain why immunotherapies have thus far only had a limited effects in AML. It’s an important step forward, but continued research and clinical trials will be needed before it can be relevant as a treatment for a patient group that is in great need of new therapies,” says Niklas Landberg, research group leader at Lund University and medical registrar in hematology at Skåne University Hospital, and one of the researchers behind the study.
The study marks a step towards more individualised cancer therapy, in which the patient’s tumour can be attacked based on its unique characteristics and defences. The work on further development and testing of the antibody will continue, with an aim to establish future clinical trials.
The team behind the study has started a spin-off company, Lead Biologics, which is now driving the commercial development of the antibody as a future medicine.
The study was carried out with funding from, among others, the Swedish Childhood Cancer Fund, Swedish Cancer Society, Swedish Research Council, ALF funding, Knut and Alice Wallenberg Foundation, Mats Paulsson Foundation, Mrs. Berta Kamprad’s Cancer Foundation (L2CancerBridge grant at CREATE Health Cancer Center) and the Cancera Foundation.
Immunotherapy is a revolutionary treatment approach for different forms of cancer. Since approval was granted for the first checkpoint inhibitors, the research community has pursued answers to explain why many patients do not respond to their treatments – and how more tumours’ defence mechanisms can be broken down. New targets, such as the mechanism now discovered, pave the way for more accurate and effective immunotherapy.
Source: Lund University
06.10.2025