News • Fewer heart surgeries, more patient deaths
Landmark study examines 'Covid effect' on cardiac surgery
The most deadly global health crisis in a century has resulted in a substantial decline in overall heart surgery volume and an unexplained increase in deaths after coronary artery bypass grafting, according to late-breaking research presented at the 57th Annual Meeting of The Society of Thoracic Surgeons.

“This study was a true herculean analysis and tour de force that showed the Covid effect on adult cardiac surgery volume, trends, and outcomes,” said Tom C. Nguyen, MD, from the University of California San Francisco. “The pandemic has changed the world as we know it, causing a dramatic drop in adult cardiac surgery volume and worsening patient outcomes.”
Dr. Nguyen and colleagues queried the STS Adult Cardiac Surgery Database from January 1, 2018, to June 30, 2020, and The Johns Hopkins Covid-19 Dashboard from February 1, 2020, to January 1, 2021. The researchers examined data from 717,103 adult cardiac surgery patients and more than 20 million Covid-19 patients in an effort to determine how the pandemic affected adult cardiac surgery on national and regional levels. “Only the STS National Database has the level of granularity, Covid variables, and longitudinal follow-up to answer the questions posed in this important study,” said Dr. Nguyen. “Our research also analyzed data by regions to get an idea of how specific areas did during the Covid pandemic.”
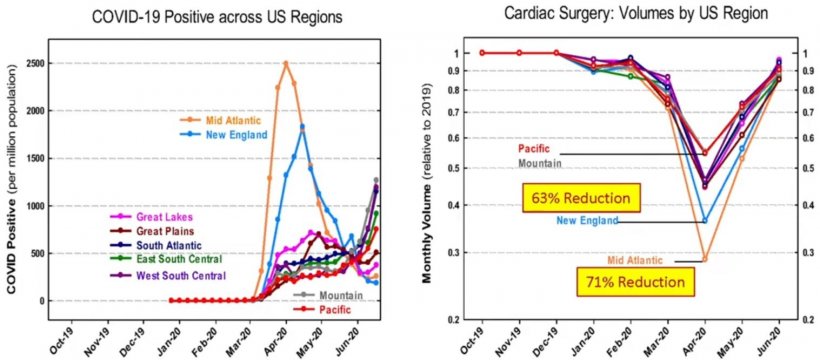
Image source: The Society of Thoracic Surgeons
According to the study results, there was a 53% decrease nationwide in all adult cardiac surgery volume when compared to 2019 and 65% fewer elective cases in the United States. Covid also impacted non-elective cases, resulting in a 40% decrease. In addition, the data showed that no matter the procedure—isolated coronary artery bypass grafting (CABG), isolated aortic valve replacement (AVR), isolated mitral valve replacement (MVR), CABG+AVR, CABG+MVR, isolated MV repair, and CABG+MV repair—there was a significant decline in case volume—54%—when compared to 2019.
Regionally, the Mid-Atlantic area (New York, New Jersey, and Pennsylvania), was among those most affected by the Covid crisis, experiencing a 71% decrease in overall case volume, 75% fewer elective cases, and a 59% reduction in non-elective cases. Another hotspot, the New England region (Maine, Vermont, New Hampshire, Massachusetts, Connecticut and Rhode Island), showed a 63% reduction in overall case volume. The researchers also found that prior to the Covid surge, the Mid-Atlantic and New England regions had excellent outcomes with an observed-to-expected (O/E) ratio of less than 1, which represents a better-than-expected mortality rate. However, during the Covid surge, there was a 110% increase in the O/E for all adult cardiac procedures and a 167% increase for isolated CABG, meaning more patients were dying than expected.
These numbers should not serve as a deterrent to patients seeking care for chest pain or other cardiac symptoms. If anything, they are a warning to get into the system as soon as possible
Robbin G. Cohen
Though the data did not directly address the cause of increased mortality, many surgeons say they currently are limited to operating on only the most urgent coronary bypass cases and patients who tend to be sicker. “These numbers should not serve as a deterrent to patients seeking care for chest pain or other cardiac symptoms,” said Robbin G. Cohen, MD, MMM, from Keck School of Medicine of the University of Southern California in Los Angeles, who was not directly involved with this study. “If anything, they are a warning to get into the system as soon as possible.”
At the time of presentation, there were 95.4 million global cases of Covid-19 with more than 2 million global deaths. The US accounted for more than 24 million cases and approximately 400,000 deaths. In the past year, this crisis has altered or halted virtually every aspect of society, and the practice of cardiothoracic surgery clearly has not been immune. The abrupt cessation of surgery in mid-March 2020 has proven to have had far-reaching implications, as the negative effects of canceled and postponed procedures on patient health outcomes now are being realized. “We clearly demonstrated that if you have heart surgery during Covid, you have an increased risk of morbidity and mortality,” said Dr. Nguyen. “No doubt that Covid hit us hard.” According to Dr. Nguyen, this study is only the first of many more “granular” analyses to come. The researchers plan to examine trends and outcomes of Covid patients vs. non-Covid patients, as well as delve more into the Covid effect on specific adult cardiac procedures such as aortic dissections.
Source: The Society of Thoracic Surgeons
02.02.2021





