Intra-aortic balloon pump pros & cons
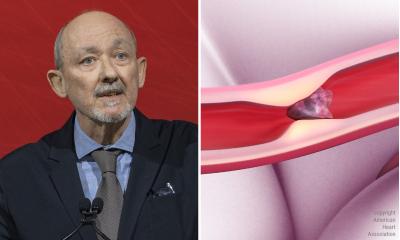
Since cardiac surgeon Adrian Kantrowitz, of the Maimonides Medical Centre, Brooklyn, first introduced intra-aortic balloon pulsation (IABP) into clinical practice in 1967 (Surg Clin North Am. 1969 Jun; 49 (3) :505 -11), the technique has been considered the method of choice for short-term mechanical cardiac support following a heart attack.

The principle is impressively simple. Connected to a helium pump, a cigar-shaped balloon is ECG triggered, folded and inserted into the femoral artery in the groin and pushed into the descending aorta to the point where the tip rests just under the aortic arch. After the left ventricle has ejected its blood into the aorta, the balloon is quickly inflated. The aorta is blocked, blood cannot flow out peripherally and so flows into the coronary arteries improving blood flow in the now relaxed cardiac muscle. Milliseconds prior to the next heartbeat the balloon is abruptly drained, creating a slight vacuum effect and making it easier for the heart to eject the blood.
The procedure had already received a class 1 recommendation in the treatment guidelines. However, only every fourth patient in cardiogenic shock is treated with this method and there is some doubt as to its effectiveness. The recommendation was recently downgraded to class 11a.
In August 2012, a randomised multicentre study was presented at the European Cardiology Congress in Munich. Out of 600 patients with cardiogenic shock (CS) after acute myocardial infarction (AMI) 301 received IABP and 299 did not. Both groups received percutaneous coronary intervention (PCI).
After 30 days, 119 patients (39.7%) in the IABP group had died and, in the control group, 123 patients (41.3%) had died. ‘The use of intra-aortic balloon counter pulsation did not significantly reduce 30-day mortality in patients with cardiogenic shock complicating acute myocardial infarction, for whom an early revascularisation strategy was planned,’ said Professor Holger Thiele, cardiologist at the Heart Centre at the University of Leipzig, representing the authors of the SHOCK-II-Trial (N Eng J Med. 2012 Oct 4;367 (14) :1287-96).
Some experts were surprised, others not – i.e. those who had not necessarily been following the class I recommendation unconditionally. Maybe simple semantics could help here. Where nothing pulsates, i.e. during cardiogenic shock, there is nothing to counter pulsate.
Meanwhile, a further study was published that examined a different patient population and collated long-term data. This study came to a different conclusion. Out of 301 patients with impaired cardiac function and severe coronary disease, 151 received high risk PCI with IABP, and 150 without. Mortality data for the entire cohort were available after a median 51 months. Overall, 100 patients (33%) died, with 42 of those in the group that had received IABP and 58 in the group that had not.
Dr Divaka Perera, cardiologist at St. Thomas’ Hospital, London, explained: ‘Elective IABP use during PCI was associated with a 34% relative reduction in all-cause mortality compared with unsupported PCI’ [Circ. 2013 Jan 15;127 (2):207-12]. Professor Marco Tubaro, cardiologist at the San Filippo Neri Hospital, Rome, put it this way: ‘Even if a reduction of mortality has not been demonstrated with IABP in association with primary PCI, the bulk of evidence and everyday clinical practice are in favour of IABP use as haemodynamic support in patients with AMI complicated by cardiogenic shock non-immediately responsive to volume expansion and inotropic stimulation.’
Professor Andreas Markewitz, Lieutenant Colonel in the German medical corps and cardiac surgeon at the German Armed Forces Hospital in Coblenz, sees another aspect. Out of all patients in the SHOCK-II-Trial only a little over a third (38%) were completely revascularised. ‘IABP is only of benefit if the heart is given a chance to completely recuperate,’ Prof. Markewitz believes. Additionally, in patients with multi-vessel disease this is often not achieved with PCI; coronary bypass surgery (CABG) is the superior procedure here.
The professor therefore believes that IABP should continue to be considered very important for cardiac surgery. ‘Soon,’ he said, ‘there will be a new, interdisciplinary S3 guideline that will confirm this.
Profile:
Since 2010, Colonel Professor Andreas Markewitz, MD has directed the Department XVII, at the Cardiovascular Surgery Clinic, German Federal Armed Forces Central Hospital, Coblenz. He gained his medical degree and specialist training in surgery at the University of Tübingen. In 1994, he wrote his habilitation and a year later he became a senior consultant at the Coblenz hospital. He qualified as cardiac surgon in 1996. The professor is very active in the German Society for Thoracic and Cardiovascular Surgery, the German Cardiac Society and the German Interdisciplinary Association for Intensive Care and Emergency Medicine.
After gaining his medical degree at the Free University of Berlin, Professor Holger Thiele specialised in internal medicine at the Leipzig Heart Centre and the German Heart Institute in his home town, Berlin. Following a research period alongside Professor Mohan Sivananthan in Leeds, UK, he became a consultant and, in 2006, senior consultant under Professor Schuler at the Leipzig Heart Centre.
03.09.2013