Networking
Improvements in efficiency and quality through digitalisation
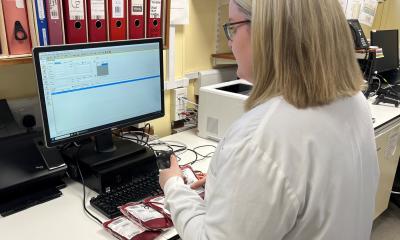
Increasing requirements for specialisation and diagnostic quality in pathology on the one hand and the importance of pathology findings for treatment planning on the other hand call for new solutions in pathomorphological diagnostics. One important starting point is the fast-paced opportunity for digitalisation along with communication systems which facilitate the storage and transfer of large volumes of data. These open up new opportunities in pathology summarised by the term ‘digital pathology’. “The term digital pathology stands for procedures which facilitate improvements in quality and improved exchange with colleagues in the same field who may have a different or special expertise in certain areas. It also serves the improvement of communication with hospitals, both internally and across larger distances,” explains Prof. Dr. Hans-Peter Sinn of the Institute of Pathology at Heidelberg University Hospital.
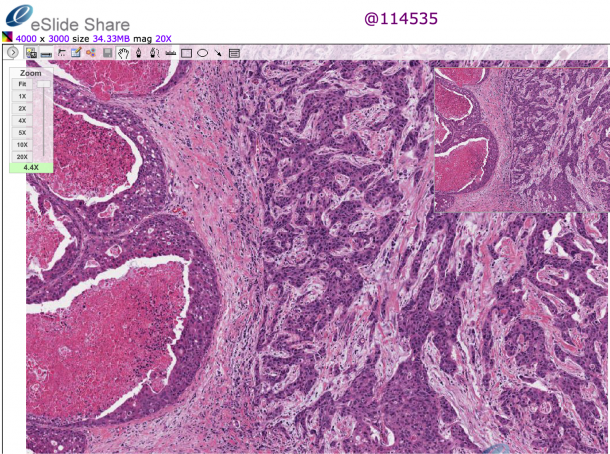

Telemedicine in pathology used to be referred to as “telepathology”. But the term only means that a diagnosis is carried out over a certain distance for conventional preparations. It has a historical background, as there were efforts in the 1990s to transmit diagnostic images via bundled ISDN lines or similar, i.e. using outdated means which have long been abandoned due to the unsatisfactory technology and limited validity. Pathology, and in particular tumour pathology, is increasingly integrating non-morphological procedures such as NGS (next generation sequencing) on which classifications are dependent. Histological preparations are now primarily digitalised and made available by the server via virtual microscopy. “The term ‘digital pathology’ not only comprises the transmission of images but also their metadata and additional information concerning the case which the pathologist can use to gain a more complex understanding than with a microscopic image alone,” explains Sinn.
The process of digitalisation is unstoppable
Digitalisation in pathology facilitates improved standardisastion, transparency and digital archiving of microscopy. But there is also another important factor. “Telemedicine in pathology allows the networking of pathologists with one another in an uncomplicated way, particularly with regards to specialised areas of expertise. There are networks for haematopathology and gynaeocopathology where content about histological preparations, research concepts or molecular procedures can be exchanged,” reports Sinn. Telemedicine not only concerns patients and individual cases (teleconsultation) but also includes continued education, quality circles, lecture series, tumour registers and reference centres.
So, is everything positive? By no means! “The process of digitalisation is unstoppable, but in the case of routine pathology has only just begun and poses particular challenges for pathology. This concerns, for instance, the lacking standardisation of platforms, image formats and interfaces of virtual microscopy with pathology- and hospital information systems. There is currently also a lack of non-proprietary solutions for the networking of subsystems for molecular pathology and immunohistochemistry.” Furthermore, financial aspects also play an important role. It would be misleading to assume that digitalisation and electronic provision of histological preparations and results definitely lowers costs per se by, for example, assuring that duplicate examinations are avoided. “This is not actually the case with digital pathology,” says the expert and substantiates this as follows: “Digitalising histological preparations or other pathological findings, making them available electronically and transmitting them if required involves higher costs. We depend on the conventional histological, immunohistological and molecular methods and then have to digitalise them in a secondary procedure. Therefore, digitalisation is a secondary, expensive step. These days it is still easier and cheaper to put samples into envelopes and send them off. The costs of digital pathology are in the high six-figure range and therefore significantly higher than exchanging preparations in the conventional way.”
The enormous amounts of data which need processing are a further problem: “Due to the microscopic resolution required the image data takes up a lot more storage space than the data stored in radiology for instance. A single histological preparation once digitalised converts into around one gigabyte of data. If we want to digitalise our entire microscopic diagnostics we would generate several hundred terabytes of data a year, and over a period of several years for routine image documentation in microscopy for just one institute would end up in the petabyte range. This is another reason why digitalisation in pathology is still a lot less common and standardised than in other areas of medicine,” explains the expert.
Sinn is essentially in favour of further digitalisastion, which he believes to be unstoppable. However, he warns against being naïve about it: “The introduction of telemedicine on a broader scale primarily improves the quality of care, and only secondarily the efficiency. In the future this will result in the opportunity to work more objectively and in a more networked manner through the increased digitalisation of medical results. The patient therefore has the potential advantage of improved care, but the higher costs and significantly increased expenditure regarding time and resources are limiting factors, particularly for pathology.”
PROFILE:
Professor Dr. Hans-Peter Sinn studied medicine at the Universites of Erlangen and Munich. He is the Head, Division of Gynecopathology, Institute of Pathology, Heidelberg University Hospital. His fields of interests are the molecular and clinical pathology of the breast and female genital tract, computer based education and postgraduate training in pathology and virtual microscopy.
17.11.2015