Hepatocellular carcinoma
Treatment without surgery, a conservative alternative
Cases of hepatocellular carcinoma (HCC), one of the most frequently occurring cancers throughout the world, are expected to increase dramatically in the next 10-15 years in Germany alone. The main reason is the increased occurrence of fatty hepatitis. Thus, in the future, interventional radiologists will also be increasingly involved in HCC patients treatment.

Two procedures in interventional radiology – thermo-ablation and chemo-emolisation – increasingly assume an important role in HCC treatment, because they offer a large variety of options and are well suited for most patients. However, there are questions: Which method should be used under what circumstances? Which indications and contraindications should be considered? We asked Professor Thomas Helmberger, Chief Physician of the Institute for Diagnostic and Interventional Radiology and Nuclear Medicine at the Bogenhausen Medical Centre in Munich, who is among the first in Germany to practice the still new method of selective internal radiotherapy (SIRT).
As the initiator and chairman of the German Society of Interventional Radiology and Minimally Invasive Therapy, Prof. Thomas Helmberger is keenly interested in advanced training in interventional radiology and intends to introduce the SIRT method into a refresher course. ‘We are still a relatively small troop of specialists and are happy to be in the front line and provide information about what we do,’ he said, smiling.
In the treatment of hepatic tumours and metastases, interventional radiology along with medical hepatology and oncosurgery are a powerful combination. On this there is general agreement on the treatment protocols for hepatic carcinoma. Based on the very well organised recommended guidelines recommendations, under the supervision of the qualified specialists it is possible to choose with certainty the correct intervention for HCC. If surgical removal of the carcinoma is impossible, the time for interventional minimally invasive procedures has arrived.
‘During the past few years, our specialty has gained increasing importance as a unique discipline all of its own. In addition to vascular medicine, it has been possible with modern technologies, as presented in the refresher course, also to play a role in oncology. In this way surgical interventions are being replaced by image-guided, bloodless procedures,’ said Prof. Helmberger.
A truly strong trend lies in radio frequency ablation (RFA) of primary and secondary liver tumours. This involves introducing a probe comparable to a puncture needle into the tumour tissue. The probe contains antennas that are extended like an umbrella in malignant tissue. A radio frequency generator is used to conduct high frequency alternating current into the antennas, which creates heat and cooks the tumour. However, the procedure has its limits he explained: ‘The heat radius of the antennas is limited to about 4 cm. This means that the tumour focus should not exceed a size of three to six centimetres and that the margins also should be easy to determine. It is not advisable to place several punctures next to one another in larger tumours. This is not only a time-consuming process, but the risk of carrying over or leaving behind tumour cells is too great.’
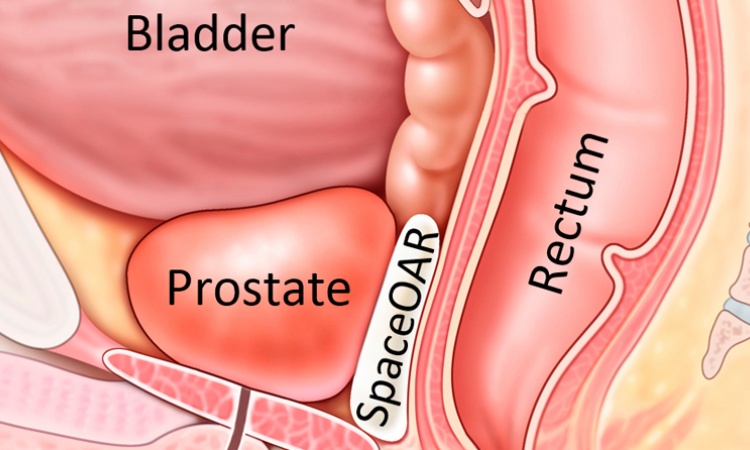
Since 2003, SIRT in Europe has been a novel treatment method that is particularly effective in diffuse, multifocal tumour formations. What is unique about this embolisation technique is the fact that the particles are radioactively enriched and thus can directly irradiate the cancer foci in the liver. The chemotherapeutic agent used in the beads is the isotope Yttrium 90. The microspheres (diameter approx. 35 µm) have a physical half-life of about 64 hours and locally achieve a high radiation effect corresponding to a dose of 200 Gy with a low range of approximately 1 cm. Yttrium 90 is injected into the entire liver via the hepatic artery and reaches even the smallest vascular branches. Metastases that are scattered throughout the liver can be optimally reached in this way.
However, the evaluation of data and study results obtained for SIRT are difficult because the method is only suitable for a limited group of patients. Treatment successes are established by a comparatively small number of cases. Prof. Helmberger explained the reason: ‘There is an important exclusion criterion for the use of SIRT and that’s liver cirrhosis. In Europe hepatic cancer almost always occurs as a result of inflammatory liver damage. While the normal liver obtains 80% of its blood and nutrient supply from the portal vein and only 20% from the hepatic artery, this relationship is reversed in liver cirrhosis. Thus, an occlusion of the hepatic artery by means of SIRT would have fatal consequences.’ Therefore, SIRT only can be used in patients who have a healthy liver, e.g. in colon cancer with hepatic metastases.
‘Furthermore, before Yttrium 90 therapy it is absolutely necessary to check whether a patient has genetic or disease-related shunts between the vessels of the liver and the lungs,’ the professor stressed. ‘If this is not detected, radiation pneumonitis can develop.’
The shunt vessels act like a direct shortcut between the hepatic artery and the hepatic vein. This means that the Yttrium particles do not first pass into the liver tissue, but flow directly into the hepatic veins. These veins transport the chemotherapeutic agent via the heart into the lung where it becomes deposited in the peripheral vessels and irradiates the lung from the inside out. Therefore, SIRT is free of complications only if it is certain that the microspheres remain in the liver after administration.
Innovative procedures such as radio frequency ablation and SIRT cannot replace the surgical removal of HCC, but do facilitate access to conservative treatment alternatives. Thus, radiological interventions represent important pioneering work in oncotherapy at the highest level to the benefit of the patients.
12.11.2009