Article • Local and elegant
Extending life with TIPS and TACE
Liver disease is widespread in Germany. It is, in fact, the most common cause of death in patients under the age of 40, with liver cirrhosis, which can develop into liver cancer, playing a major role here.
Report: Karoline Laarmann
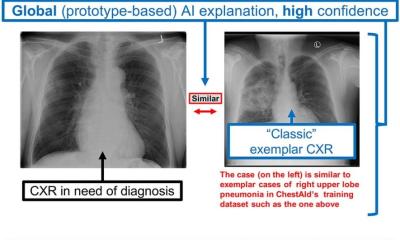
These days, modern, comprehensive treatment concepts are unimaginable without interventional radiology, for liver cirrhosis as well as liver cancer. Prof. Dr. Christian Stroszczynski, Director of the Institute for X-ray Diagnostics at the University Hospital Regensburg, introduces two of the most important liver interventions for advanced stages of liver disease which all radiologists should be familiar with – TIPS and TACE.
The reason why liver disease is on the rise in this country is mainly down to an unhealthy lifestyle: too much alcohol and a bad diet are amongst the most common risk factors. The results can be alcoholic fatty liver disease or non-alcoholic fatty liver disease, which can develop into liver cirrhosis. Hepatitis B- and C viruses can also lead to liver cirrhosis. A further risk factor, though this is quite rare in developed countries, is the mycotoxin Aflatoxin.
Prof. Stroszczynski works at the Liver Centre of the University Hospital Regensburg, in close cooperation with his colleagues from the fields of gastroenterology, hepatology and surgery, as: “The best possible decision on treatment can only be taken by an interdisciplinary team.” Radiological interventions are always an inherent part of the treatment spectrum.
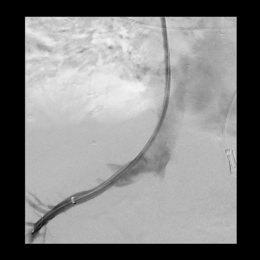
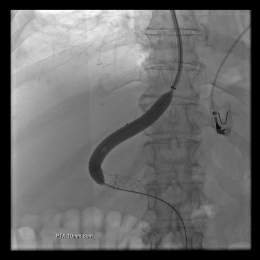
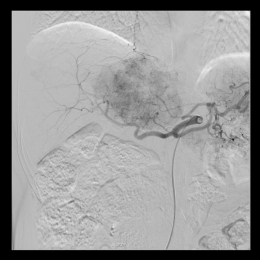
One procedure for the treatment of portal hypertension which has near enough replaced the surgical procedure was even invented in Southern Germany: the transjugular intrahepatic portosystemic shunt, known as TIPS. The procedure was first introduced for clinical use at the University Hospital Freiburg (Nöldge et al 1992). TIPS insertion is indicated for patients with advanced liver cirrhosis to prevent life threatening complications such as ascites or bleeding oesophageal varices. A shunt is used to create a connection between the portal vein system and the hepatic veins.
“At the beginning, TIPS was accepted with great enthusiasm, before almost disappearing from the scene again,” reports Prof. Stroszczynski. “Only when some convincing studies on the procedure were produced which showed that it improves the prognosis significantly did it prevail in the end.” These days, 80 new TIPS interventions are carried out minimally invasively in Regensburg alone each year.
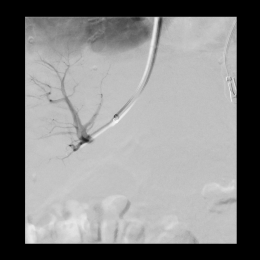
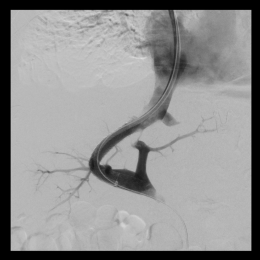
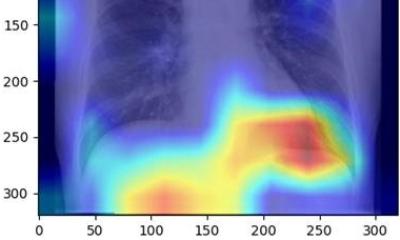
TIPS cannot prevent the development of a hepatocellular carcinoma (HCC). In most cases, liver cirrhosis is the breeding ground for the development of liver cancer. “Unlike for other cancerous diseases, chemotherapy does not help with this type of cancer,” explains the radiologist. “This means that, apart from novel immune procedures with strong side effects, there is no drug treatment which we can offer these patients. Transarterial chemoembolisation, also known as TACE, however, is a very elegant local procedure as it only rarely results in the usual side effects such as hair loss, nausea or vomiting.”
This is because chemotherapeutic agents are injected directly into the tumour so that only those cells are damaged which are supposed to get damaged – which in turn means that a very high dose can be administered locally. Along with cytotoxins, small particles are administered into the hepatic arterial blood vessels to obstruct these and to decrease the blood supply of the tumour. Therefore, along with palliative efforts, TACE is often also used for downstaging of an HCC prior to surgical resection or liver transplantation.
The good thing is that there is a lid for every pot, i.e. a suitable procedure for each tumour for these liver interventions, and that they can also complement one another
Christian Stroszczynski
The big breakthrough for TACE came through the randomised study carried out by Llovet et al. in 2002, which showed that the one-year survival after chemoembolisation compared to conservative therapy increased to 82%. The method is primarily used for tumours which are too large or numerous for curative treatment.
“Although we cannot help in these cases, we can alleviate,” explains Christian Stroszczynski. “The good thing is that there is a lid for every pot, i.e. a suitable procedure for each tumour for these liver interventions, and that they can also complement one another. This helps us to extend the median survival time after diagnosis of liver cancer, which used to be around six months, to two years.
Profile:
Prof. Dr. Christian Stroszczynski took up his position as Chair of Radiology and Director of the Institute for X-ray Diagnostics at the University Hospital Regensburg (UKR) in October 2010. Prior to his move to Regensburg he was assistant director and senior consultant at the Institute for Diagnostic Radiology at the Carl-Gustav-Carus University Dresden for four years. In May 2016 he was elected as Chair of the German Society of Interventional Radiology and Minimally Invasive Therapy (DeGIR).
29.11.2017