Infectious diseases
Developing vaccines and nanotechnology
Vaccination remains one of the most efficient strategies against infectious diseases, often being the best protection against infections such as hepatitis B, or influenza. European Hospital reports on expert reviews of vaccines in the pipeline and the potential of nanomedicine given during the Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC) annual meeting in Seville.
Report: Mélisande Rouger

Vaccine science has evolved greatly over the past few years, according to Dr Carlos Martín from the Medical Faculty, University of Zaragoza: ‘There’s been a huge advance not only preventing infectious diseases but also chronic diseases such as cancer. The hepatitis B vaccine, for instance, has significantly lowered the incidence of liver carcinoma and, with the papilloma vaccine, we will see less and less cases of cervical cancer in the coming years.’
Clinic trials
Most commonly, new vaccines in development use viruses or new generation of adjuvants to improve immunisation. They can use adenoviruses such as MVA, virus-like particles, purified proteins or nanoparticles.
It is essential to conduct efficacy clinical trials and new technologies, such as transcriptomics, could be used as potential correlates of protection to accelerate the development of a new vaccine, Martín explained. ‘We usually have to wait 25 years for a vaccine to be developed and bringing it to the market costs between 500 and 800 million euros. In the 80s, the discovery phase was extremely long and clinical trials lasted about five years,’ he said. ‘We should be able to reduce the time of clinical trials with new technologies.’
Combined vaccines reduce HIV
HIV is an important but complex area of innovation. Researchers have worked for the past 20 years on a prevention cure for AIDS, first with inactivated viruses, and then with vaccines trying to improve T-cell response by using Adenovirus and Poxvirus. According to Martín, recent studies have shown that combining those two vaccines reduced HIV infection by 30%.
Over 100 of malaria vaccine candidates, studied in animals, and dozens of clinical trials exist for malaria. Adjuvants are just as important in the equation. A study conducted in more than 15,000 infants and young children showed that malaria vaccine RTS S candidate reduced disease over four years of follow-up. Protection is low – only in about 30% of the vaccinated – and reduces within a year, but approval is under study. ‘That would be the first time that a protection vaccine against malaria would be brought to the market,’ he said. Due to the human challenge, the context of vaccine development for malaria has changed tremendously.
TB: Respiratory transmission route
Things are also changing for TB, a disease responsible for 1,000,000,000 deaths in the past two centuries, according to an article recently mentioned in Nature.
The BCG candidate has been around for over 100 years and is used worldwide. The problem is that TB’s main route of transmission is respiratory, which BCG does not cover. In 1993 a mycobacterium bovis triggered a very resistant TB epidemic in Spain. The strain showed an increased expression of the phoP gene. The unusual outbreak killed 114 individuals and was highly transmissible by aerosol route. This spurred the creation of the MTBVAC candidate, following recommendations by the 2005 Geneva consensus criteria that two stable independent mutations (phoP and fadD26) should be used for live vaccines.
Some of the newest developments include vaccines against cytomegalovirus, dengue and Japanese encephalitis, RSV and, last but not least, Ebola. The latter actually serves as a model of accelerated vaccine development, according to Martín. ‘This epidemic caught us by surprised because of its scale. But there were already candidates in macaques, so things went quickly.’
The rVSV-ZEBOV – recombinant vesicular stomatitis virus and the ChAd3-ZEBOV – chimpanzee adenovirus 3 had already been used in clinical trials in Switzerland, the USA and Germany before December 2014. There are now Vaccine Phase 3 efficacy trial designs in Liberia and Sierra Leone. ‘By comparison, we’ve been in the developing process of a malaria vaccine for over 25 years; and in Ebola we’ve shorten this period to one year!’ Martín said.
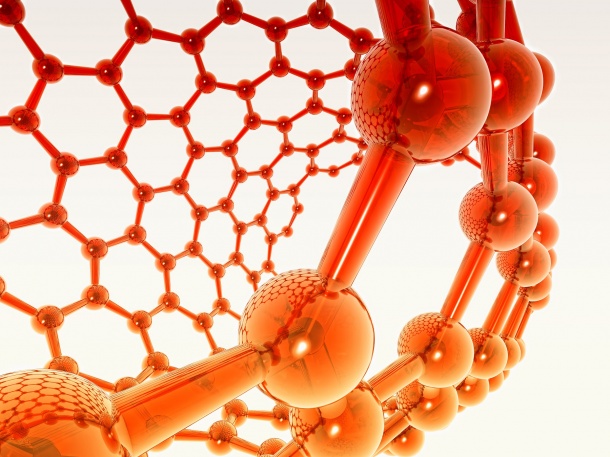
Dr Eduard Torrents from the Catalan Bioengineering Institute observed the potential role of nanomedicine, which applies nanotechnology tools such as atomic force microscopy, scanning tunnelling microscopy and dip pen nanolithography to infectious diseases.
Nano-delivery products are helpful
Nanoparticles (NPs) are particularly helpful in drug delivery because they are soluble and bio available, and decrease immunological reactions, Torrents explained: ‘They deliver a predetermined dose while decreasing the frequency of administration, enabling drugs delivery locally and precisely, and minimise secondary effects, and liberate two or more components in combined therapies.’
There are currently 44 nano-delivery products on the market, including some for fungal infections and oral and perioral infections, as well as 18 pharmaceutical products, one of which is designed for fungal infections.
This figure is expected to grow as labs express an increased interest in the field. The nanotechnology market represented 73 billion dollars in 2011 and is expected to grow to 131 billion in 2016, at a rate of +12.5% a year. In 2016 nano products will represent 10% of all sales in pharma industry.
To advance NPs use, Torrents recommended that nano scientists should get away from the evidence concept, understand that pharmacokinetic concepts in NPs are different and conduct infection trials in animal models. There should be functional and safety studies, which shouldn’t follow the patterns of classical pharmacology studies.
‘Challenges remain in the detection of infectious agents, penetration of the hematoencephalic barrier and antibiotics resistance. Metallic NPs are very promising,’ he concluded, ‘and we hope to be able to use them for vaccination, and open the oral and pulmonary routes for drug delivery.’
Profile:
Carlos Martín is Professor of Microbiology at the Faculty of Medicine, University of Zaragoza, and a member of the Advisory Committee of Tuberculosis Vaccine Initiative (TBVI). With more than 25 years of experience in mycobacterial genetics he, and his team, aim to develop novel TB vaccines and vaccination strategies to improve protection against pulmonary TB. He is currently working in collaborative TB research projects with research groups in Europe and Latin America. Previously, Martín worked as permanent researcher at the Pasteur Institute in Paris, and he has published more than 100 international publications on TB. Since 1992 his TB research has continuously received national and European Union funding. The professor also belongs to CIBERES, a research network on respiratory diseases of the Spanish Ministry of Health (Instituto de Salud Carlos III).
04.09.2015