Article • Evaluation
Calculated therapy is the objective
At a recent focus meeting held in Berlin by the Association of Accredited Laboratories in Medicine, Dr Andreas Weimann, managing director at the Laboratory Berlin – Charité Vivantes Services, spoke of the challenges that laboratories working with hospitals face due to the management of pathogens and the diagnosis of infections.

‘We are clinging to red tape. Instead of prevention, our focus is on those who are already ill,’ Weimann explains, in the “Five Bad Habits of Healthcare” drafted by the World Economic Forum 2012. Demographically, the focus is increasingly on older, multi-morbid patients who are particularly exposed to infectious agents due to their complex clinical pictures. Weimann refers to patients who have had organ transplants as an example. There are no reference values for this group. ‘Can you spontaneously state the reference value for liver function tests in a 75-year-old, immune-suppressed liver transplant patient? We don’t know it!’ Yet it is precisely these kind of questions that clinicians want laboratory medics to answer.
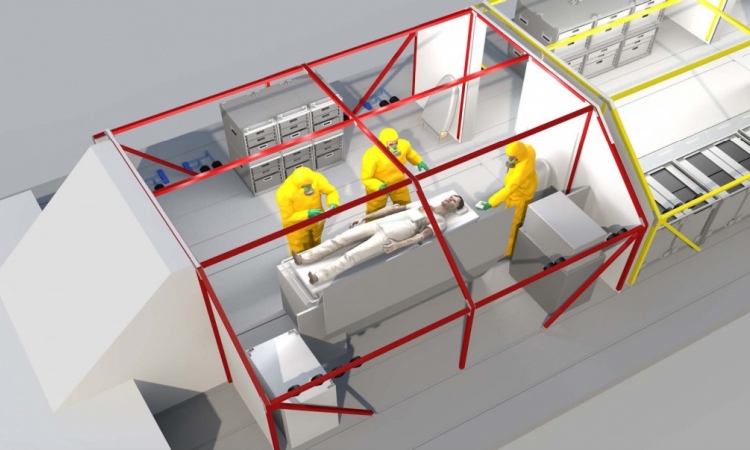
Is an infection local or is it sepsis? Is it bacterial or viral? Should I administer effective, anti-infective chemotherapy or not? What is the severity? Can I make a prognosis? Weimann emphasises that, particularly in the field of intensive care medicine, one should be realistic enough to anticipate that some patients will not survive. Effective screening of pathogens and the effectiveness of medication with regards to selected biomarkers can help doctors in their decisions as to whether treatment should be continued or whether life-preserving measures should cease – from a cost perspective, as well.
Such screening should ‘…buy the intensive care medic time to actively wait,’ Weimann points out. Sometimes, such a comprehensive, sufficient diagnosis also allows the doctor to ‘do nothing for a day’. It also makes significant contributions towards cost efficiency, allowing better control over the development of multi-resistant pathogens.
With these multi-resistant pathogens in mind, Weimann talks of the current practice of antibiotics prescriptions in Germany: 85% of all antibiotics are administered in veterinary medicine. Of the 15% prescribed in human medicine only 0.5% are used in intensive care medicine. Weimann calls this a ‘topsy-turvy world’.
One large problem in anti-infectious therapy is the high rate of wrongly prescribed antibiotics, i.e. unnecessary prescriptions and those inappropriate for the respective pathogens. ‘The current best practice appears to be to shoot sparrows with cannons,’ Weimann says wryly.
Affected patients are typically not male, aged around 20 and with a weight of 70kg, such as described in text books but old and sick
Andreas Weimann
Over the last ten years, in cooperation with medical company Sysmex, the Berlin Laboratory, at the Charité, has been developing the sepsis ‘Intensive Care Infection Score’ (ICIS), which is based on cellular values and aims to facilitate a better prognosis.
A combination of 10 readings, evaluated and scored, could then for instance be displayed over an intensive care patient’s bed. This would allow doctors to quickly orient their strategy based on the respective prognosis. The ICIS is available 24/7/365 in all locations in the hospital, but requires specific staff training as to the score values used in on-going treatment.
Weimann quotes an example from the Charité. When a sepsis patient is treated with antibiotics it needs sufficient drug monitoring. In the case of multi-morbid, intensive care patients particularly, the doctor will usually prescribe not just one antibiotic but a combination. The objective of therapeutic drug monitoring (TDM) is sufficient control of pathogens, as well as the prevention of toxic effects. Weimann points out that affected patients are typically not ‘male, aged around 20 and with a weight of 70kg, such as described in text books’ but ‘old and sick’, with several potential sources of infection arising from various access ports to the body.
Furthermore, the interactions between various different types of medication that most people are prescribed due to multi-morbidity must be taken into consideration. ‘Nobody can do this. But what we can do is determine the concentration from the serum.’ This means different concentrations and different effective dosages in different patients. Sufficient drug monitoring and close cooperation between clinicians and laboratory staff enables the development of a personalised TDM record for each individual patient.
Calculated therapy is the objective. The development of a ‘house standard, adapted to the existing mix of patients’ is the method of choice. The interdisciplinary working group ABx has developed a web-based programme of recommendations (www.dgai-abx.de) to treat infections in intensive care and emergency medicine. The ABx programme offers evidence-based recommendations while taking into consideration the national and international guidelines for calculated antimicrobial therapy.
‘Why are we making these huge efforts?’ the expert asks at the end of his lecture, before concluding: Antimicrobial Stewardship Concepts (AST) are integral to sepsis treatment. Consistent AST appears to reduce time spent in the hospital, reduces antibiotics prescriptions and lowers the cost per intensive care patient. ‘The evaluation of severe infections requires cooperation between many different laboratory disciplines – methodically as well as organisationally,’ Weimann confirms.
27.04.2016