Blood vessel lining cells control metastasis
Scientists from the German Cancer Research Center in Heidelberg and from the Medical Faculty Mannheim of Heidelberg University treated mice with a combination of a low-dose metronomic chemotherapy and an antibody against Ang-2, a regulatory protein of the blood vessel lining cells. The treated animals had significantly less metastases.
Cancer patients without overt metastases appear to be "tumor-free" upon surgical removal of the primary tumor. Yet, metastatic spread of tumor cells may already have occurred at the time of surgery. Many tumor patients are consequently treated with chemotherapy after surgery to fight metastasis. This may be necessary in patients with detectable metastases, but what kind of more gentle treatment options can be offered in patients without overt metastasis?
"It's a major dilemma for many tumor patients after surgery: Should they opt for a high-dose chemotherapy with all its devastating side effects? Or should they just wait-and-see and possibly live with a higher risk of metastatic disease?" asks Professor Augustin. His laboratory at the German Cancer Research Center in Heidelberg and at the Medical Faculty Mannheim of Heidelberg University is studying the mechanisms of metastasis with the goal to develop more gentle supportive adjuvant therapies for tumor patients without detectable metastases following surgery of the primary tumor. Towards this end, the scientists focus on novel findings that suggest a much more active tumor-promoting role for endothelial cells, the cells lining the inner wall of blood vessels.
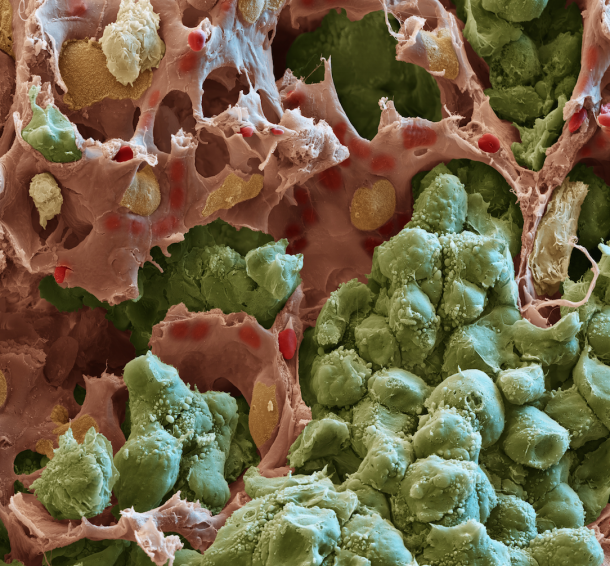
Tumor cells engage nearby blood vessels to grow new capillaries that nourish the tumor and thereby facilitate its growth. This process, called angiogenesis, is well understood and has already led to clinical application 10 years ago. Albeit still limited in efficacy, angiogenesis-inhibiting drugs have become part of standard tumor therapy supporting the efficacy of established chemotherapies.
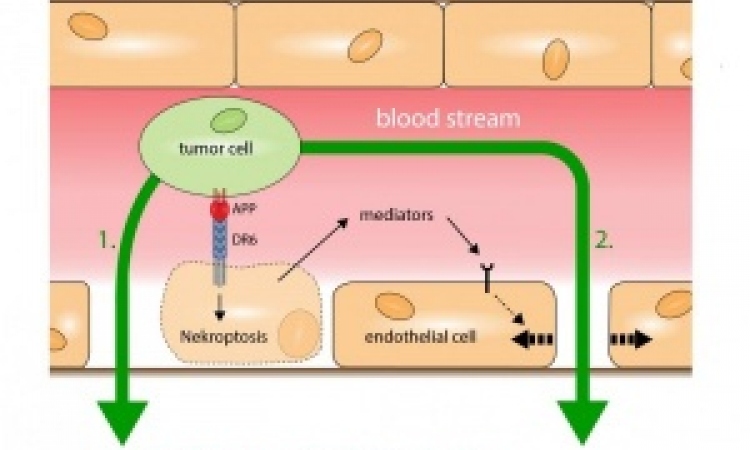
The classical concepts of angiogenesis consider the endothelial cells within tumors as a rather passive cell population that merely reacts in response to growth factors released by the tumor cells. Yet, more recent discoveries suggest a much more active role of endothelial cells during tumor growth than has been anticipated so far. The scientists in Augustin's laboratory consequently pursued preclinical tumor therapy experiments, which were aimed at not just blocking angiogenesis, but to also suppress the production of tumor-promoting growth factors in endothelial cells. They focused towards this end on the vascular growth factor Angiopoietin-2, which is produced by endothelial cells and does not just control angiogenesis, but acts as a key responsiveness factor for endothelial cells.
The researchers grafted breast or lung tumors in mice, allowed the tumors to grow to small size and removed these tumors surgically - essentially mimicking the situation in a human tumor patient in which the tumor is surgically removed as soon as possible after diagnosis. The mice appeared after surgery to be apparently 'tumor-free'; yet, metastatic cells had already seeded from the small tumors. The mice were upon surgery consequently treated with various forms of chemotherapy as well as with a blocking antibody targeting Angiopoietin-2.
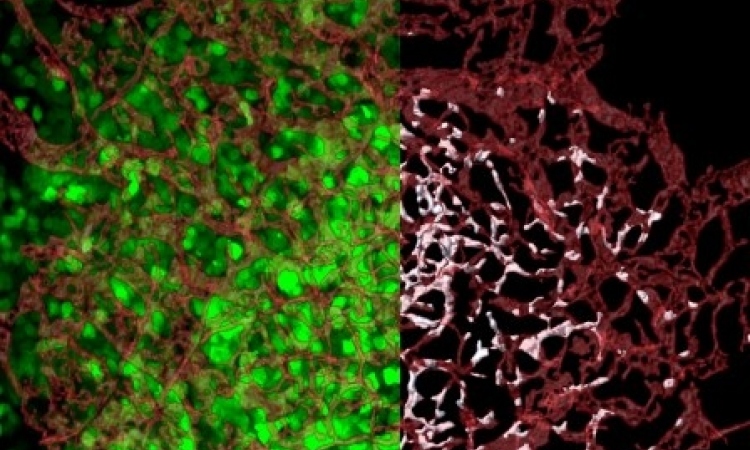
Surprisingly, while neither form of chemotherapy had any effect on the growth of these seeded metastases, Angiopoietin-2 antibody treated mice had significantly less metastases in the lungs and in the bone and survived longer than untreated control mice. This therapeutic effect was enhanced by combining the Angiopoietin-2 antibody with a so-called metronomic chemotherapy: In this kind of therapy, chemotherapeutic drugs are given continuously at much lower dose as in the classical high-dose chemotherapy. Mice treated with such combination therapy survived significantly longer than mice just treated with the Angiopoietin-2 antibody.
Based on these surprising therapeutic effects, the scientists initiated experiments aimed at unraveling the underlying molecular mechanisms of the novel combination therapy. These analyses showed that Angiopoietin-2 is not just affecting angiogenesis, but controls at the same time the production of tumor promoting growth factors in endothelial cells. These endothelial-derived factors stimulate the recruitment of tumor-promoting macrophages into the tumor. The blockade of Angiopoietin-2 reduced the recruitment of these macrophages.
The second branch of the combination therapy, the low-dose metronomic chemotherapy, was similarly found to exert its therapeutic effect through a novel, hitherto unrecognized mechanism: The metronomic chemotherapy turned out to not primarily target the tumor cells, but to act on the recruitment of yet another tumor-promoting cell population from the bone marrow.
"This novel combination therapy simultaneously targets multiple pathways contributing to metastasis" explains Professor Augustin, "On the one hand, we inhibit the growth of new blood vessels in metastases. On the other hand, we block the recruitment of macrophages, which elicit an inflammatory response and thereby contribute to shaping the conductive soil on which metastases can grow". Cautiously, Augustin adds: "Obviously, we don't know if the findings of this study can be translated directly to human tumor patients. Yet, the fundamental insights into the mechanisms of metastasis will pave the way for the rationale translation of these preclinical discoveries into clinical application."
Source:
Press Release: German Cancer Research Center
Kshitij Srivastava, Junhao Hu, Claudia Korn, Soniya Savant, Martin Teichert, Stephanie S. Kapel, Manfred Jugold, Eva Besemfelder, Markus Thomas, Manolis Pasparakis und Hellmut G. Augustin: Postsurgical adjuvant tumor therapy by combining anti-Angiopoietin-2 and metronomic chemotherapy limits metastatic growth. Cancer Cell 2014, DOI 10.1016/j.ccell.2014.11.005
07.01.2015