© phonlamaiphoto – stock.adobe.com
News • Exploring potential and limitations
Bedside bioprinting: the future of regenerative medicine?
In a collaborative article Gorka Orive, a researcher in the UPV/EHU’s NanoBioCel group, explores the potential and limitations of 3D bioprinting as well as the challenges it faces in the area of tissue regeneration.
Researchers say the problems of poor printed cell density need to be overcome, each tissue needs to be provided with the corresponding characteristics, and this direct bedside biofabrication needs to be achieved.
Regenerative medicine uses cells that are injected, grafted or implanted into a patient to exert a desired therapeutic effect, such as the healing of traumatic wounds. However, some of the key challenges to success involve getting the therapeutic cells to reach their destination effectively, without loss of survival and function, and ensuring that they are integrated into the tissue. To make the most of the potential of cell therapy in this type of medicine, it is important to adopt, adapt or develop better tools to produce high-quality, cell-based products using various 3D printing techniques.
Getting that cell concentration to increase artificially with these technologies remains a challenge that the technology has to tackle in order to be able to adapt its applicability to tissues much better
Gorka Orive
In collaboration with renowned scientists in the area of biomaterials and bioprinting from Harvard University and the Technical University of Denmark, Gorka Orive, a researcher in the NanoBioCel Group, has published an article in the journal Science. In discussions with Yu Shrike Zhang (Harvard University) and Alireza Dolatshahi-Pirouz (DTU), with both of whom he works closely, “we wondered how this technology (which is widely recognised in the field and for which there is a considerable amount of literature) could be taken to a higher level: how improved applications in the field of regenerative medicine could be implemented”, explained Orive. In this respect, after outlining the potential of this technology and the limitations and challenges that lie ahead, the article proposes some ideas that could be used to achieve a better outcome.
The researchers concluded that one of the most pressing challenges needing to be overcome is related to cell density: “When cell structures are manufactured by means of additive printing, the cell load per quantity of printed material remains low. And this is definitely a problem, because that's not how the body works. Our body has a much higher cell density. Getting that cell concentration to increase artificially with these technologies remains a challenge that the technology has to tackle in order to be able to adapt its applicability to tissues much better,” said Orive.
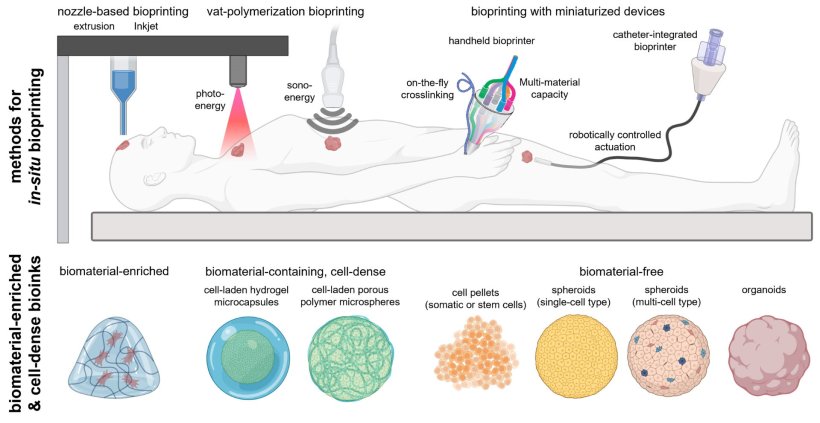
Image source: UPV/EHU; Gorka Orive
Another of the essential aspects for progress that they highlight is related to the characteristics of the tissue to be regenerated; the researcher maintains that “muscle tissue and liver tissue, for example, do not have the same characteristics or functionalities, nor do they even have the same cell or tissue shape. In other words, the bioprinting process is neither identical nor the equivalent”. In the researcher's opinion, “getting 3D printing technology to adapt to each type of tissue would be a major breakthrough”.
The researchers also cite the need “for bioprinting to be brought closer to the clinical setting. It should not remain in the laboratory, it is important for it to be brought closer to the clinical approach, to regenerate the patient’s affected tissue directly, in situ or ‘at the bedside’”.
Orive believes that “although the challenge is huge, everything that favours the implementation of all these advances going forward will undoubtedly be very positive. It is difficult, but so was the application of stem cells, for example, and they are now used in the clinical setting in specific areas for tissue regeneration, for the treatment of certain chronic diseases, etc.” The researcher argues that “science is taking steps forward. If you don't dream about what you want to achieve, you are not likely to achieve it”. Orive admits that “this does not mean that what we have put our names to will become reality tomorrow, but it does mean that in the journal Science at least, as well as in the scientific evaluation made by other experts, it is considered to be an interesting insight in the field”. All these advances emerge out of basic research, “out of the effort of dreaming about how to succeed in applying this technology in the clinical setting. Solid research projects, grounded in good basic research, need to be developed in multidisciplinary teams”, he concluded.
Source: University of The Basque Country
09.11.2024