Bayer Healthcare’s 7th European Diabetes Nursing Symposium
Meike Lerner reports
In November, European diabetologists converged on Leverkusen, Germany, to discuss current practices in diabetic management of Type 1 and Type 2 in adults, as well as new technologies, procedures and the need for patients’ education.

Specialist diabetes nurse Sari Härmä-Rodriguez, from the Diabetes Centre of the Diabetes Society in Finland, emphasised that, along with treatment management, psychological support is significant, reminding participants at the annual Bayer event in Leverkusen that behind all the guidelines and treatment targets there is always an individual with his/her own needs. There are many medical devices to treat Type 1 diabetes, she said, ‘But, to get the best results, personal education plays an important role. The measurement of blood glucose, for example, only makes sense if the patient can interpret the results and therefore change behaviour. If patients do not know what to do with the results, they lose the interest of measuring at all.’
Future technologies, such as direct feedback via a mobile phone, might alleviate those processes in the future. Another point is that, although insulin pens and pumps significantly increase the quality of life of Type 1 diabetics, there still is a lot to learn – from patients and physicians. According to Sari Härmä-Rodriguez many healthcare professionals do not know, for example, how to use and recommend insulin pumps.
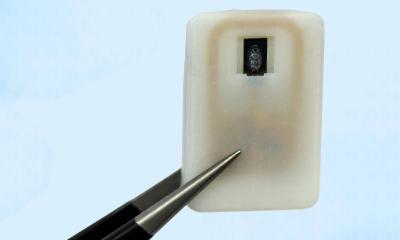
Whilst that can be solved by education, in the future an artificial pancreas could become an option for diabetics. However, despite efforts, a healing option for Type 1 diabetes is not on the horizon. As long as no potential weapon is found, diabetes remains a huge psychological burden. ‘Type 1 patients suffer twice as much from depression as healthy people and often have severe eating disorders as well as cognitive dysfunctions. Additional mental stress is caused by the omnipresent fear of hypoglycaemia and other phobic disorders as well as by social aspects like restrictions in working and private life,’ the Finnish expert explained, imploring colleagues to provide psycho-social support to avoid a diabetes-burnout.
She also appealed for a re-think on adult diabetics’ education and use of peer-support and personal coaching methods: ‘Adults have a long history of the disease, have lived many therapy options and tried a lot of therapy approaches. So, during their lifetime, they develop a kind of education resistance that only can be overcome by a personal and individualised coaching.’
In his lecture, John Nolan, Professor for Endocrinology and Biochemistry at Trinity College, Dublin, Ireland, supported her: ‘In the first line, diabetes treatment should fit to the patient -- even more important because expenditures for the illness will soon overcome national health budgets. In the near future, approximately 10% of the population will be affected by diabetes. Those figures will definitely have a strong impact on the extent and continuity of care,’ he explained, pointing out that Type 1 diabetics will be hit even harder from budgetary cuts because, due to the predicted diabetes epidemic and global awareness of type 2 patients, they will slip out of focus.
Urging lobbyists and politicians to create a balanced awareness of both types and that consistent guidelines be established, he said: ‘Only half of all EU-member States have a national diabetes plan, so I request all parties involved – from patients to caregivers – to fight for their rights and urge governments to support a national plan.’
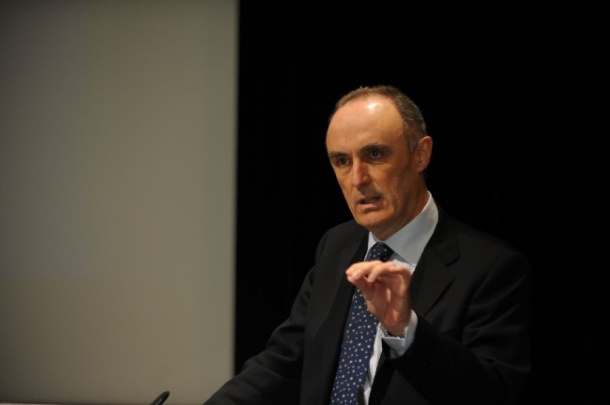
Angus Forbes, Professor for Diabetes Coaching and FEND-Chair of Diabetes Nursing, Great Britain, echoed the need for coaching: ‘The current diabetes epidemic has the power to cave in healthcare systems across Europe, destabilised recent advances and negatively affect future developments. A huge challenge for care providers will be to develop evidence-based approaches that will feed this need.’ Such approaches must be more efficient and more effective models to support behaviour and diabetes self-management.
He also sees the need for a more personalised therapy and suggested a shift from the average person to the individual: ‘Treatment needs to be more selective and targeted. This includes a huge challenge for nurses, because models of care will become far more complex and, in future, there will be a greater complexity in decision-making. There will be more therapy options to chose from, a wider metabolic management, the consideration of obesity management etcetera.’ Solving this dilemma, Prof. Forbes concluded, will mean improving primary prevention, self-care support and the care system as a whole.
29.12.2010