Advancing POC diagnostics
Engineer Frédéric Breussin, expert in microfluidics for diagnostics and life sciences and Microfluidics Project Manager for Yole Développement, explains how new technologies can enable the development of more sophisticated point-of-care testing
Improvements in microfluidics and detection technologies are beginning to expand the range of point-of-care diagnostics beyond simple blood chemistry tests to sophisticated immuno-assays and molecular diagnostics. Though yet to see much adoption in European hospitals, these point-of-care (POC) diagnostics are coming into use in the USA, initially in emergency rooms and ICUs where fast results are most critical.

But, gaining full advantage from some of these potentially game-changing innovative technologies will require re-thinking some conventional ways of doing things.
Despite major investment and big strides in microfluidics technology, in 2010 the sales of POC diagnostic devices still only reach about US$200 million, not including reagents. However, the capability for fast, low cost testing for many more conditions is spurring growth, with demand on track to average 38% annually for the next five years, to become a US$770 million market by 2014, according to the Yole Développement latest analysis of market trends (Report: BioMEMS 2010) as developers and potential users of the technology learn to integrate disparate technologies into integrated systems for simple, low cost tests, and to focus on the right markets with real benefit to patients and medical practitioners.
Due to recent advances in the microfluidics technology used in research labs, it is now possible to make low cost polymer slides that can actively pump, mix, separate and heat and cool samples and reagents through complex pathways and test regimens. This makes possible a growing selection of disposable slides or cartridges to do chemical tests of drops of blood in ~10 minutes or less, for US$4 to US$20.
Commercial tests are now available for multi-chemistry blood analysis, blood gases, electrolytes, cardiovascular diseases, inflammation and diabetes from various suppliers. Companies such as Biosite offer systems for immunoassays to diagnose cardiac conditions in about 15 minutes. The polymer microfluidics systems bring the cost of the device down to a few dollars, bringing total cost, with reagents, IP and marketing, to US$30-US$100 per test.
However, it has taken some time to find the right applications with the right balance of medical benefit, efficiency and cost to get real benefit from these new technologies. The compelling advantage of true POC diagnostics is, of course, fast results right where they’re needed, where getting test results in minutes in an emergency can enable immediate critical treatment of things like heart attack, stroke, drug overdose, or sepsis, and cost is not a major issue. However, only a handful of these critical applications are available, which has limited early adoption of the technology.
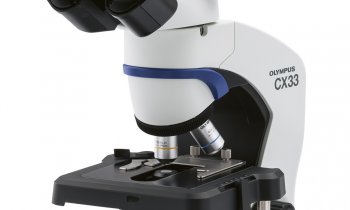
Intensive care units and emergency rooms are finding real advantage from instant blood test results in the USA. Abbott Point of Care, for example, sells some 20 million units a year of its bedside i-STAT blood chemistry tests with a handheld reader, which give medical personnel immediate information on blood chemistry for US$4 to US$20 a test set cartridge, using capillary forces to drive the sample through analysis, and measuring changes with thin film electrodes.
i-STAT systems are used by Baystate Health System, in Springfield, Massachusetts, for example, for >100,000 blood gas tests a year out of some 600,000 ambulatory visits and 140,000 emergency intakes.
In other cases, it may require changes in the system to capture the benefits of immediate POC information. Sometimes the true medical benefit to the patient of obtaining a diagnosis in minutes, not days, may be marginal, but the operational benefits to the system of increased efficiency and reduced costs might be huge – from eliminating the constant shuffling of many blood samples and test results back and forth between the lab and dialysis centre, say, or eliminating the need for doctors to schedule additional time for follow-up phone discussions of results with every patient who has lab tests. These benefits may not be so obvious, and they might require significant changes in established practices of sending samples to the lab and later receiving the results.
The most promising coming application for the more specific and sensitive nucleic-acid-based tests now becoming possible with low cost microfluidics is testing for infectious diseases, which offers calculable economic benefit over the old immunoassay systems by identifying the genetic differences in the pathogens that determine how resistant or virulent they are, and speeding up diagnosis from days to hours, to begin treatment sooner and to prevent the disease spreading through the population.
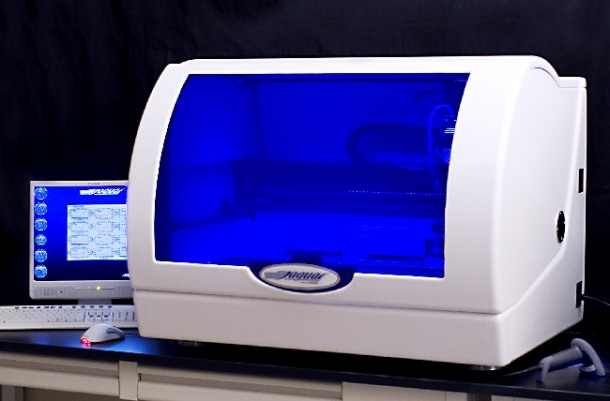
Automated lab equipment that can run these tests for infections like HIV, hepatitis, flu or MRSA in several hours in the hospital lab, is now available from most of the major players, though the systems remain relatively large and expensive. Acquisition of small suppliers by the medical majors, such as the BD Diagnostics’ acquisition of HandyLab, will help bring these completely automated systems into wider distribution.
29.12.2010