Advances in MRI/ultrasound fusion biopsy
Widely considered a safe procedure for targeted tissue sampling, the fusion of MR and ultrasound images for prostate biopsy purposes is quickly gaining ground among radiologists.

Currently, fusion technology is a major research focus at many radiology centres: MRI/ultrasound fusion biopsy is being implemented, new transducers are designed, the potential of elastography and other procedures are combined – and results are highly promising. This is good news for patients since in Germany alone every fourth male is affected by prostate cancer and more than 60,000 new cases are recorded annually.
European Hospital asked one of the pioneers of fusion biopsy, Professor Thomas Fischer MD – Managing Senior Resident at the Radiology Department in Charité Campus Mitte and Head of the Interdisciplinary Ultrasound Centre at Charité, Berlin – about the challenges and prospect of the procedure and experiences in the use of a Hitachi ultrasound system for fusion biopsy.
Prof. Fischer: ‘Hitachi Real-time Virtual Sonography – HI-RVS – has been around for more than ten years. Originally developed for radiology, in the meantime HI-RVS has conquered urology. What makes this system unique? Interestingly, the very fact that the system has been on the market for some years and uses a biplanar transducer, the EUP-CC531, which combines the advantages of conventional core biopsy with fusion ability, as well as elastography and contrast imaging. Due to its shape, this transducer is ideally suited for prostate examinations.
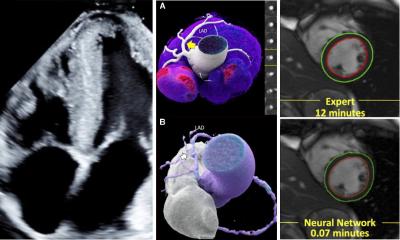
‘While it achieves the image quality of a state-of-the-art transducer, its anatomy fusion is faster and easier to understand, particularly for operators who are not so familiar with this procedure. The specific design of the probe, double curved array orthogonally positioned, allows an easier understanding of the prostate anatomy as seen on the MRI image, because it matches ultrasound planes easily with sagittal and axial views of the prostate MRI – a major advantage.’
Hitachi was the first to introduce elastography. Do you use this technology in prostate biopsies?
‘Absolutely! Despite all efforts the images can never be compared one to one, one reason being that the pressure exerted by the transducer deforms the prostate. This deformation limits comparability. However, in order to hit the tumour I need to move in the correct plane. Since the lesion may be very small, around 5 mm, I use elastography to localise the aggressive stiff tumour tissue.
‘With MRI we navigate to the tumour site plane, and then we use procedures such as elastography or contrast-enhanced ultrasound – CEUS – to fine-tune the lesion positioning. And here the biplanar transducer also plays an important role. During actual examinations I even turn off MRI for some time, to be able to see the second ultrasound plane, orthogonal to the one I was previously using, which gives me a better idea where exactly the tumour is located. If I can see the tumour in two image planes I can hit it precisely with the needle.’
Is fusion helpful for other organs?
‘Fusion can be very helpful in liver studies although unfortunately, in this country, it is rarely used in this area because of diverging professional interests. On the international level, fusion is the domain of radiologists because you do have to be familiar with CT and MRI. For example, a patient presents with skin cancer. CT staging is performed to detect metastases. This is done on the basis of a particular protocol that encompasses one-time administration of a contrast agent. If a suspicious lesion in the liver is detected you cannot tell – due to the single-phase procedure – whether it’s a cyst, a haemangioma or metastasis. This is where fusion comes in, especially in lesions difficult to see in Ultrasound.
‘The radiologist takes the patient and CT data to the ultrasound lab, where he injects a contrast agent into the region of interest, fuses the CT and US image data and then can see whether it’s a cyst, haemangioma or metastasis. Fusion of CT and US images, as described in our discussion, offers much more precise diagnostic possibilities. Moreover radiation dose can be saved and the results can be verified either right away with a biopsy or with a third modality, namely MRI.’
‘Right now we are talking about detection only, meaning diagnostics. We’ll begin with CT staging, an established standard procedure, to see if and where we are dealing with metastases. That is impossible with ultrasound. If a suspicious lesion is detected in the liver, or the spleen, which cannot be clarified with a single-phase CT study, then fusion comes in to help.
‘In short: The other phases are added to the CT scan and by looking at the portal or any later phase we can tell – unambiguously – whether the suspicious lesion is a melanoma or a metastasis. With these data the case can be discussed by the Tumour Board and everyone present, no matter from which medical discipline, can understand the facts and findings. Why? We see the CT images plus the contrast-enhanced ultrasound image from the same plane.
‘That’s not all. What about treatment? I have to verify whether the patient responds to the therapy or not. That means looking at exactly the same spot in exactly the same planes, which is pretty difficult with ultrasound; but when I can call up the CT data with the reference lesion, I can compare the data, avoiding when possible a new CT examination of the patient (radiation dose saving).
‘Identifying and differentiating lesion in CT staging – that’s is the domain of this fusion technology.’
Profile:
Professor Thomas Fischer has directed ultrasound diagnostics at the Radiology Institute at the Charité Clinic in Berlin, since 2007. Since 2009 he has also headed the ultrasound research laboratory at the Charité, which specialises in testing new ultrasound procedures and techniques in complementary studies.
18.11.2013