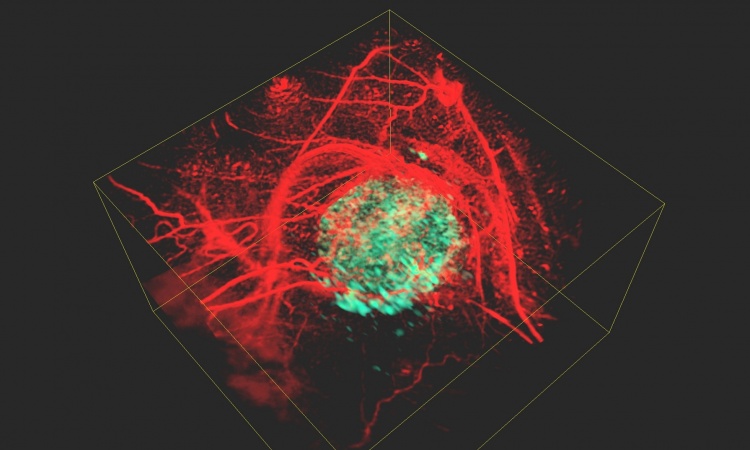
© Rajewsky lab, Max Delbrück Center
News • Spatial transcriptomics and ECM imaging
3D insights into the tumor microenvironment
Researchers in Nikolaus Rajewsky’s lab at Max Delbrück Center combined high-resolution, single-cell spatial technologies to map a tumor’s cellular neighborhoods in 3D and identify potential targets for personalized cancer therapy.
They describe their findings in two separate papers in “Cell Systems.”1,2
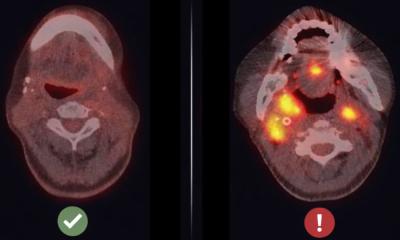
Understanding not just what cells are present in a tumor, but where they are located and how they interact with other cells around them – their cellular neighborhoods – can provide detailed insights that help doctors determine which treatments or therapies might be most effective for a specific patient. An international research team led by the Berlin Institute for Medical Systems Biology at the Max Delbrück Center (MDC-BIMSB) combined spatial transcriptomics in 3D and extracellular matrix imaging to gain unprecedented detail about the inner workings of an early-stage lung tumor. The proof-of-concept study was published in “Cell Systems”.
So not only do we know what cell types are present, we know how they are grouped with their neighbors, and we could begin to understand how tumor cells rewire non-malignant cells at the tumor surface to support tumor growth
Tancredi Massimo Pentimalli
“Tumors are complex ecosystems where tumor cells live in close contact with the surrounding extracellular matrix. They interact with many other cell types,” says Professor Nikolaus Rajewsky, director of the MDC-BIMSB, head of the Systems Biology of Regulatory Elements lab and senior author on both papers. “The data we can obtain now in tumor tissues from a patient are becoming so precise and comprehensive that we can computationally predict the molecular mechanisms which are driving phenotypes. This is new and fundamentally important for making personalized medicine a reality.”
Transcriptomics documents what RNA is being actively expressed in cells, which indicates the activities the cell is engaged in and reveals the cell types present in a sample. Spatial transcriptomics does this but for individual cells to build a 2D map. The team got early access to the CosMx instrument from the company NanoString, which does this at extremely high resolution – 1,000 different RNA molecules can be detected at one time, compared to traditional methods that identify just a handful of molecule types at once. The team analyzed 340,000 individual cells from the lung tumor, identifying 18 cell types.
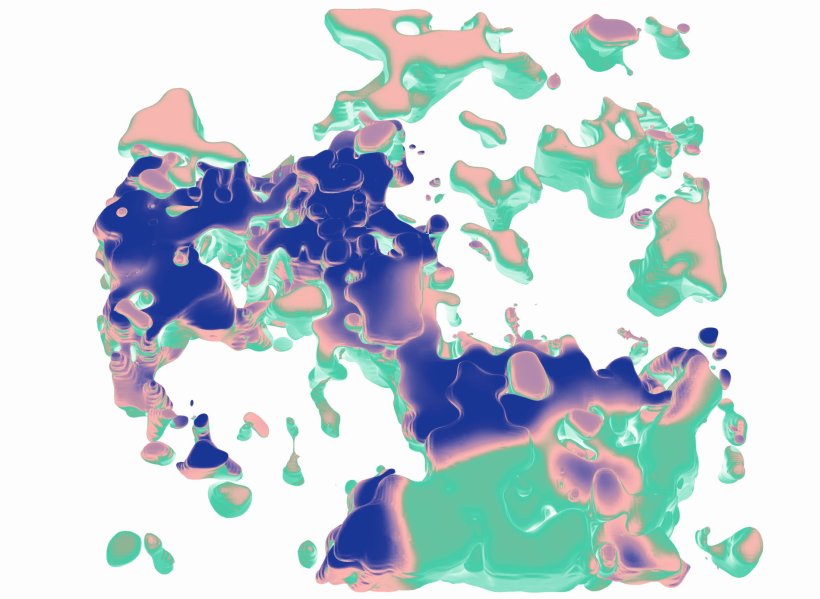
The 3D analysis was powered by a new computational algorithm, STIM, which aligns datasets to reconstruct 3D virtual tissue blocks. “We realized that spatial transcriptomics datasets can be modeled as images,” says Dr. Nikos Karaiskos, a postdoctoral researcher in the Rajewsky lab and co-corresponding author of the second “Cell Systems” paper describing STIM in detail. Leveraging imaging techniques, STIM marries the fields of computer vision and spatial transcriptomics. The team worked closely with Dr. Stephan Preibisch, a former principal investigator at MDC-BIMSB who is now at Howard Hughes Medical Institute’s Janelia Research Campus in the U.S., to bring this collaborative effort to fruition.
They then worked with the Systems Biology Imaging Platform in Mitte to apply a separate imaging technique, called second harmonic generation, to map elastin and collagen in cellular neighborhoods, which in the lung are the main extracellular matrix constituents. Areas with more elastin were healthier, while those with more collagen surrounded the tumor cells, which indicates harmful tissue remodeling.
“So not only do we know what cell types are present, we know how they are grouped with their neighbors, and we could begin to understand how tumor cells rewire non-malignant cells at the tumor surface to support tumor growth,” explains Tancredi Massimo Pentimalli, MD, the first paper's first author who is pursuing a PhD in the Rajewsky Lab and the Berlin School of Integrative Oncology at Charité – Universitätsmedizin Berlin.
This is pathology 2.0 – not just looking at the cells under a microscope to make a diagnosis, but bringing molecular insight to the clinic
Tancredi Massimo Pentimalli
But the analysis did not stop there. The team was able to understand precise phenotypes – for example, if fibroblasts, which form connective tissue, were activated and remodeling the tissue or not. They were also able to listen in on cell-to-cell communication and determine how tumor cells were blocking immune cells from entering the tumor. “This immune suppression mechanism is well-known and suggests immunotherapy would help,” Pentimalli says. “Immune checkpoint inhibitors would reverse the suppression and then you have this army of immune cells that are already in position ready to attack. It was exciting to see how our approach identified this dynamic and could help direct a personalized immunotherapy plan.”
Notably, these key insights were only possible with data in 3D – in 2D it was impossible to distinguish between the tumor and other immune cells embedded in the tumor surface.
The beauty of this approach is that, while very high-tech, it starts with a routine tissue sample found in any pathology lab. For this study, the group used a tissue sample of a lung tumor that was several years old, preserved with formalin and embedded in paraffin wax – the standard method pathologists use to preserve archival tissues. “We were able to extract all this wealth of molecular information from one very thin section of a sample that has been sitting around at room temperature for years,” Pentimalli says. “This is pathology 2.0 – not just looking at the cells under a microscope to make a diagnosis, but bringing molecular insight to the clinic.”
Now that the proof-of-concept has been established, the team plans to apply the approach to larger datasets. They are currently working on 700 samples from 200 patients and collaborating with Dr. Fabian Coscia, who leads the Spatial Proteomics Lab at Max Delbrück Center, to integrate protein activity into the analysis.
Source: Max Delbrück Center; text: Laura Petersen
25.04.2025