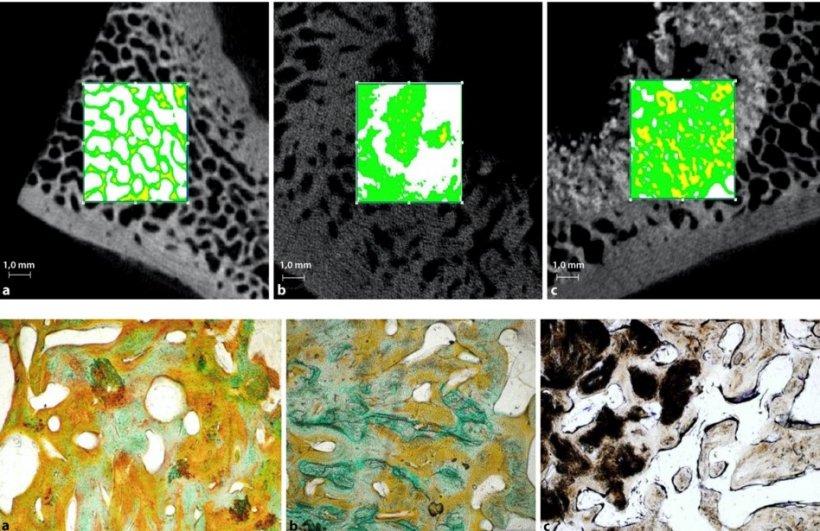
Source: Koob S, Gravius S, Wirtz DC: Der Orthopäde 2017: 158-167
Article • Bioprinting
3D biocomposites can repair large bone defects
Loosening hip implants can cause major damage to the bone and a simple replacement won’t suffice to carry the load during movements. “To solve this problem we have to turn to innovative technologies such as bioprinting. Scaffolds are required that – while adapting slowly – offer long-term stability,” says Professor Dr Dieter Wirtz, Director of the Department of Orthopaedics and Trauma Surgery at the University Hospital Bonn, Germany.
Report: Sonja Buske
For several years tissue engineering procedures have been available to repair smaller bone defects in orthopaedics and trauma surgery. Bone replacement material enriched with cells can replace bone in non-load carrying areas and if the defect is less than 3 cm in diameter. Larger defects in load carrying areas, e.g. pelvis implants, however continue to be a major clinical challenge. “In these cases the defect has to be repaired in a way that offers stability in order for the bone to carry load,” Professor Wirtz explains and adds that “today, our only option is metal which has a limited life span.” Thus, he is looking to develop a biomaterial to replace bone tissue. First animal tests have yielded promising results.
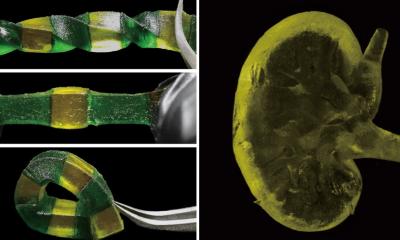
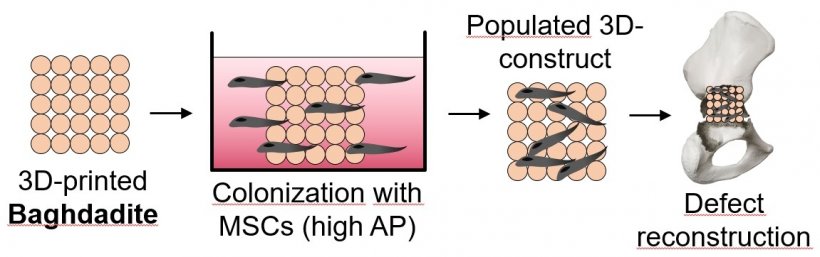
Professor Wirtz’ research partners in the biomedical group of the University of Sydney are helping along: they developed a baghdadite-based calcium-silicate ceramic material with different degrees of porosity which offers the required stability in 3D bioprinting. “This is a good material to repair load-carrying defects. Since the ceramic is inorganic, bone cells have to be added,” Wirtz explains. His team developed a method to insert stem cells into baghdadite: “First, the material is created in the 3D printer. In a second step it is immersed in a kind of stem cell bath. This allows the stem cells to dock onto the material, enter through the pores and merge with the material. Then the biocomposite can be implanted into the damaged bone.”
Source: Professor Dieter Wirtz
Biocomposites in large animal tests
Professor Wirtz is planning further research into biocomposites. In a large animal test project the material will be tested in sheep – which are well suited since they live in flocks. In a previous test with sheep, larger defects were caused in the animals’ bones and repaired with hip implants. “The results were positive. We are now preparing a project application testing cell-based biocomposites in one group of sheep and metal in a control group. We need at least eight sheep per group in order to be able to gain reliable results.”
Since the animals have to live for at least nine months in a flock the result won’t be available before late 2022. If the large animal tests yield positive results, the next step will be a controlled clinical study in humans.
“Every year, 440,000 implants are used in Germany. None of them is stable. Each implant loosens over time. Being able to repair bone defects with biomaterials rather than metal would be enormous clinical progress”, says Professor Wirtz.
The surgeon is open to new approaches and calls on scientists, companies and physicians alike to contribute their brain power: “It would be very good if the two steps – 3D printing and attaching cells – could be done in one step. Every idea that helps improve our method is highly appreciated!”

Profile:
Professor Dr Dieter Wirtz has been Director of the Department of Orthopaedics and Trauma Surgery at the University Hospital Bonn, Germany, since 2006 and Managing Director of the Surgery Centre of the University Hospital Bonn since 2008.
In addition, he is President of the German Society for Orthopaedics and Trauma Surgery (Deutsche Gesellschaft für Orthopädie und Unfallchirurgie – DGOU) and the German Society for Orthopaedics and Orthopaedic Surgery (Deutsche Gesellschaft für Orthopädie und Orthopädische Chirurgie – DGOOC). In 2019, Professor Wirtz received the Edgar Ungeheuer Award of the German Society for Surgery (Deutsche Gesellschaft für Chirurgie).
27.12.2021