News • Overdiagnosis
Screening has had “little impact” on falling breast cancer deaths
But overdiagnosis has steadily increased over time
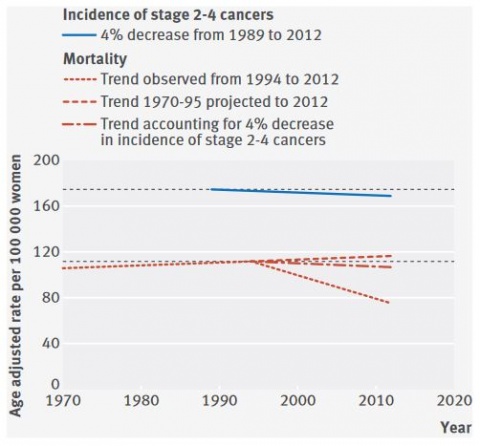
Breast screening in the Netherlands seems to have had a marginal effect on breast cancer mortality over the past 24 years, suggests research in The BMJ. Their findings show that screening would be associated with up to 5% reductions in breast cancer mortality in women aged 50 and over, whereas improved treatments would be associated with a 28% reduction. And they point out that overdiagnosis “has steadily increased over time” with the extension of screening to women aged 70-75 and with the introduction of digital mammography.
Since 1989, women in the Netherlands aged 50-75 have been invited to mammography screening every two years. In 1997, screening was extended to women aged 70-75 and digital mammography was introduced after 2006. The last evaluation of the screening programme, published in 1993, suggested moderate decreases in the incidence of some categories of advanced cancer from 1989 to 1997. So a team led by Philippe Autier at the International Prevention Research Institute in France, set out to update the incidence of different stages of breast cancer among women of all ages in the Netherlands from 1989 to 2012. They then estimated numbers of deaths from breast cancer that were avoided because of screening, and measured breast cancer overdiagnosis (number of breast cancers that would have never been detected during a woman’s lifetime in the absence of screening).
The researchers found that, after 24 years, screening would be associated with 0 to 5% reductions in breast cancer mortality in women aged 50 and over, whereas improvements in treatment would be associated with a 28% reduction. Furthermore, they say that overdiagnosis has steadily increased over time, with the extension of screening to women aged 70-75, and with the introduction of digital mammography that is able to detect increasingly smaller breast tumours, most of which are of unknown clinical importance. They estimate that about one third (32%) of cancers found in women invited to screening in 2010-12 and about half (59%) of screen detected cancers would be overdiagnosed.
The researchers highlight some study limitations that could have influenced the results, but conclude that the Dutch mammography screening programme “seems to have little impact on the burden of advanced breast cancers, which suggests a marginal effect on breast cancer mortality. About half of screen detected breast cancers would represent overdiagnosis,” they add.
Source: The BMJ
06.12.2017