News • Research
Unravelling the mystery of non-alcoholic fatty liver disease
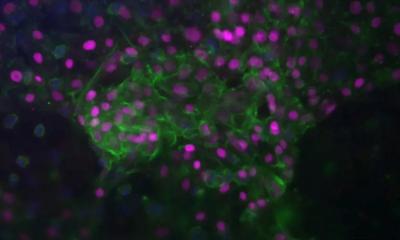
Another piece in the puzzle that is non-alcoholic fatty liver disease has been solved by a University of Queensland researcher in a step towards developing treatments for a disease that affects about one in every five Australians. PhD student Laurence Britton has discovered a pivotal mechanism by which iron is able to make the liver more vulnerable to the injury and metabolic dysfunction that precedes the disease.
University of Queensland

Faculty of Medicine Professor Darrell Crawford said Dr Britton’s discovery was an important step in combating a deadly time bomb that affected an estimated 5.5 million Australians. “With our growing obesity epidemic and no known cure for non-alcoholic fatty liver disease, an increasing number of people are sitting on a silent killer,” he said. “There may be symptoms such as fatigue, pain or weight loss – or no symptoms at all. The sufferer may not be aware that they have the disease until it has progressed to liver cirrhosis or liver cancer.“
Fatty liver disease involves an abnormal accumulation of fat, causing inflammation, scarring and an increased susceptibility to liver cancer. Previous research has shown that fat cells, iron and insulin are all major players in the disease, but the exact nature of their influence on each other has confounded medical researchers – until now.
Dr Britton found that iron reduced the availability of the protective hormone, ApoE, which is involved in fat regulation and insulin resistance. He said this finding provided another clue as to why obesity and type II diabetes are significant risk factors for non-alcoholic fatty liver disease, and gave researchers a target for future therapeutics. “Currently there is no standard treatment for the disease, with doctors instead treating the underlying conditions such as obesity and diabetes,” he said. “Understanding the modulating role of iron gives us a definite starting point from which to map the development of fatty liver dysfunction. Each element of dysfunction provides an opportunity to develop a new treatment to block the process and prevent disease progression.”
Source: University of Queensland
02.07.2018