Trends in image-guided therapy
Advanced MRI for the assessment of articular cartilage lesions and follow-up of cartilage repair tissue
In the sixth in his series for European Hospital, Professor Stefan Schönberg (left) of the Institute of Clinical Radiology and Nuclear Medicine (IKRN), University Hospital Mannheim, Medical Faculty of Mannheim, University of Heidelberg, invited colleagues from Mannheim and Vienna for a round-table discussion on:

Articular cartilage lesions caused by trauma are a very common finding which are seen most often in the knee, but are also found in the hip, elbow and ankle joint. Cartilage lesions may become symptomatic by pain and will almost inevitably lead to osteoarthritis. Since cartilage is a relatively avascular structure and has, once it is injured, only very limited capability to heal spontaneously, various surgical interventions for cartilage repair have been developed over the past years such as abrasion, microfracture, allograft transplantation and autologous chondrocyte implantation (ACT) or matrix-associated autologous chondrocyte transplantation (MACT).
Autologous chondrocyte implantation (ACI) and matrix-associated autologous chondrocyte transplantation (MACT) are advanced cell-based orthobiologic surgical techniques that are increasingly used in the treatment of isolated post-traumatic full-thickness cartilage defects, especially in the knee in younger patients. The aim of these techniques is to produce repair tissue that substitutes hyaline cartilage and becomes incorporated into the healthy surrounding tissue over the course of time in order to restore joint congruity. In the long term, it is hoped that this will prevent the progression of articular cartilage lesions to osteoarthritis.
For the classic ACT technique, chondrocytes are isolated from small pieces of cartilage that are obtained arthroscopically from a non-weight-bearing area of the knee. The extracellular matrix is removed by enzymatic digestion, and the cells are then cultured. When a sufficient number of cells have grown, these chondrocytes are implanted into the chondral defect with the use of a periosteal patch. To address the problem of cell dedifferentiation during in vitro expansion further improvements in tissue engineering have contributed to a new generation of ACT techniques, where cells are stimulated to build up an autologous matrix or cells are combined with bioresorbable materials: matrix-associated autologous chondrocyte transplantation (MACT). These biomaterials secure the cells in the defect and promote their proliferation and differentiation. The major potential complications of ACT and MACT are delamination of the transplant, periosteal hypertrophy, arthrofibrosis and transplant failure. The MACT procedures have shown a reduction in the number of complications in particular for delamination and hypertrophy which were mainly associated with the periosteal flap in classical ACI.
Magnetic resonance imaging (MRI) is a non-invasive tool for the evaluation of the morphologic status of cartilage that provides complementary information to arthroscopy. It is not only performed preoperatively to define the exact size and extent of the (osteo)chondral defect, but also throughout the postoperative period to evaluate the success of implantation, the process of healing and to identify possible complications. It thereby serves as a valuable tool in the processes of diagnosing the defect at the time of the initial injury, guiding the surgical planning and evaluating the results after surgery.
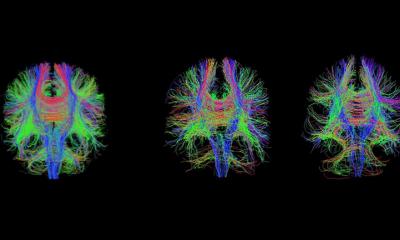
However, MR imaging of the articular cartilage is challenging, especially due to two reasons: cartilage is a thin structure (with a maximum thickness of about 4-5 mm of the patellar cartilage) and has curved surfaces. However, technologic advances in high-field imaging (with 3 Tesla and even 7 Tesla MR scanners) and coil development allow acquiring images with an excellent spatial resolution and 3-D-sequences with isotropic voxels allow excellent image postprocessing.
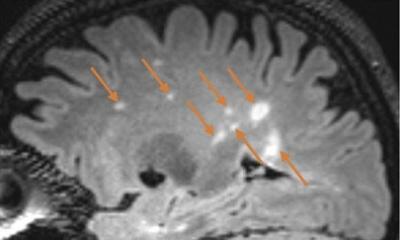
MRI with standard sequences allows a non-invasive assessment of articular cartilage with respect to cartilage morphology. The most useful sequences that provide nice visualization of cartilage are proton-density (PD) and T2-weighted (w) fast spinecho (FSE) as well as 3D spoiled gradient echo (SPGR) or fast low-angle shot (FLASH) sequences with fat suppression being very useful to visualize cartilage pathology. While cartilage has a very bright signal in 3D-SPGR and FLASH sequences that often limits the visualization of subtle cartilage pathologies, PD-w and T2-w FSE sequences show cartilage internal pathology very nicely since cartilage has an intermediate signal intensity with higher contrast in these sequences. Intermediate-w FSE sequences with a mixed PD-T2 contrast might provide even higher intrinsic cartilage contrast. In addition to these sequences, the 3D double echo steady state sequence (3D DESS) is also often used for cartilage imaging as it nicely detects cartilage lesions. By using these sequences preoperatively, the size, shape and extent of chondral / osteochondral defects can be exactly visualized and evaluated. After surgery, the degree of defect filling by the repair tissue, the integration of the transplant into the surrounding cartilage and subchondral bone, the condition and surface of the graft and the underlying bone can be nicely assessed. Also an MR-based assessment of cartilage thickness and volume as surrogate marker of a possible developing osteoarthritis is widely accepted.
It is assumed that the cartilage repair tissue undergoes three postoperative phases: the proliferative phase, the transition phase (between weeks 7-12) with formation of a type 2- collagen-matrix and the maturation phase (between week 13 up to 3 years) with formation of a hyaline cartilage-like tissue.
MRI assessment should contain the evaluation of the signal intensity of the graft, the thickness of the repair tissue in comparison to the healthy surrounding tissue (cartilage congruity), the signal intensity of the subchondral bone, displacement or delamination (of parts) of the graft, the interface between the graft material and the surrounding tissue and hypertrophy of the graft. By standard MRI, the graft signal will equal normal cartilage signal intensity approximately one year after transplantation. Subchondral bone oedema is commonly seen after transplantation, but should have been dissolved after approximately nine months to one year post ACT /MACT.
However, by MRI it is not only possible to characterize cartilage morphology and cartilage volume and thickness, but also to assess the biochemical characteristics of cartilage tissue, a field in which many research efforts are going on these days.
Advanced MR methods for the definition of the biochemical ultrastructure of cartilage that provide useful supplemental information about the histologic and biochemical contents of healthy cartilage and reparative tissue are mapping of T1rho and T2 values and delayed gadolinium-enhanced MR imaging of cartilage (dGEMRIC).
The T2-relaxation time (multi-echo, spin-echo (SE) T2 relaxation) reflects the integrity, content and orientation of the collagen fibres and the hydration status. Damage to the collagen-proteoglycan-matrix and an increase in water content in degenerative cartilage increase the T2 relaxation time. Several studies were able to show elevated T2-values in patients with osteoarthritis. Additionally, by evaluating separate zonal layers information on the type of cartilage (hyaline or hyaline-like) can be provided. In healthy cartilage, an increase of T2 values from the deep to superficial cartilage layer is observed. Animal studies with histological correlation have demonstrated that the zonal increase of T2 values can be regarded as a marker of hyaline or hyaline-like cartilage structure after cartilage repair procedures in the knee.
T1rho-relaxation time has only recently been proposed as an alternative parameter to assess biochemical changes in cartilage. The T1rho-parameter probes the slow motion interactions between motion-restricted water molecules and their surrounding. The extracellular matrix of articular cartilage restricts motion of water molecules. Changes to the extracellular matrix, such as proteoglycan loss, are therefore reflected in measurements of T1rho.
dGEMRIC is a MRI technique based on the use of an MR contrast agent that reflects the proteoglycan (glycosaminoglycan) content within the cartilage. It measures early biochemical changes within morphologically intact cartilage that may reflect early cartilage degeneration or maturation of cartilage repair tissue. The technique uses the electrostatic interaction between the negative charges on glycosaminoglycans and the negative charges on Gadolinium diethylenetriamine pentacetic acid (Gd-DTPA2-) to measure the distribution of glycosaminoglycans within cartilage. The local amount of Gd-DTPA2- within the cartilage matrix is inversely proportional to the local concentration of glycosaminoglycans. Healthy regions of cartilage show a low Gd-DTPA2- concentration, whereas abnormal cartilage regions have higher concentrations. Contrast medium is injected intravenously and after a delay period of two hours that allow the contrast agent to diffuse within the cartilage T1-measurements are performed. The images are used to calculate T1 maps that reflect the distribution of Gd-DTPA2-: areas of low T1 represent regions of low glycosaminoglycan (high concentration of Gd-DTPA2-).
Several recent studies at 1.5 T and 3 T and even first studies at 7 T have not only assessed the above described morphological parameters, but also biochemical ultrastructural characteristics of articular cartilage transplants in order to more exactly assess the outcome of surgical cartilage repair. dGEMRIC typically shows a reduced postoperative concentration of glycosaminoglycans within the graft tissue which then gradually increases over time. In several follow up studies, global T2-values seem to show no significant difference between sites of healthy cartilage and cartilage repair tissue, whereas initial results suggest that cartilage repair tissue shows a reduced zonal increase of T2-values compared to healthy tissue, indicating that the cartilage is altered and presumably not hyaline articular cartilage. Zonal assessment of T2-values therefore might be sensitive enough to characterize the maturation of cartilage repair tissue over time.
Over the last years, research efforts in the field of morphological and biochemical cartilage imaging with newly available technical developments seem to have turned cartilage imaging into ‘ in vivo functional cartilage imaging’ . The described techniques are helpful in the assessment of patients with cartilage defects prior cartilage repair and allow a non-invasive follow-up of patients after modern surgical cartilage repair techniques such as ACT and MACT.
01.03.2009