Therapies for damaged intervertebral discs
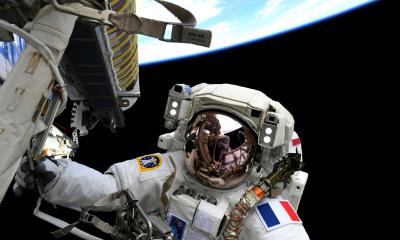
‘No large incision, no scalpel and no sutures: Radiologically guided, minimally invasive procedures can help many patients with chronic pain when conservative procedures don’t work,’ said Professor Siegfried Thurnher, head of the Department of Radiology and Nuclear Medicine at Vienna’s Hospital of St. John of God.
Picture: Hospital St. John of God, Vienna
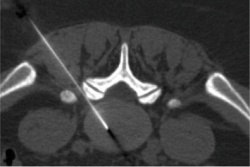
The main focal area is the spine. ‘Interventional radiology can precisely access the area where the pain originates and can, for example, administer ozone to the intervertebral discs or inject bone cement into the vertebrae to repair fractures, or fix metal or plastic sleeves in the dorsal area of the spine.’
Interventionel Radiological Olbert Symposium (IROS)
At the recent congress of the German, Austrian and Swiss (DeGIR, ÖGIR, SSCVIR) Associations for Interventional Radiology (IROS 2014) held in Salzburg this January, various sessions focused on pain therapy.
Florian Streitparth MD, from the Radiology Institute at the University Clinic Charité in Berlin, Germany, spoke on the treatment of pain caused by herniated discs and disc degeneration with so-called intradiscal procedures. The basic principle: Removal and cauterisation of the discal tissue to reduce pressure and relieve painful nerve compression.
Most important intradiscal procedures:
• Percutaneous laser-disc compression (PLDD): The nucleus of a herniated disc is shrunk using a laser beam
• Intradiscal Electrothermal Therapy (IDET): An electro-thermal probe is guided into the disc and heated to 700 Celsius
• Automated percutaneous lumbar discectomy (APLD): The disc nucleus is extracted via aspiration.
• Percutaneous laser discectomy: Water in the disc nucleus is evaporated by laser, which reaches temperatures of up to 6000 Celsius.
• Chemonucleolysis: The disc nucleus is liquefied with the help of an enzyme (chymopapain) and then aspirated.
Some of these procedures must still be considered as experimental, the radiologist explains. Initially the entire range of conservative procedures, i.e. medicinal treatment as well as physiotherapy, heat therapy and electrotherapy should be exhausted before one of these new procedures is used, Dr Streitparth emphasised, concluding: ‘At the moment, the evidence of success for these intradiscal procedures is not yet that promising. However, with good patient selection the procedures will become a good option.’
The intradiscal procedures must be on a par with well-established and very effective therapies. There is much evidence regarding the effectiveness of medicinal therapy, he points out. There is also periradicular therapy (PRT), i.e. percutaneous infiltration of the nerve roots with pain medication and similar procedures.
‘PRT and other, similar procedures are of low impact and strain and effective at reducing pain in around two thirds of patients,’ explained Dr Bernhard Oder, Head of the Department of Nuclear Medicine at the Vienna’s Hospital St. John of God. In Austria, crystalline corticosteroids are also being used for treatment, he added. However, in Germany crystalline corticosteroids have not been licensed for infiltrations to the spine. German radiologists are therefore hoping for support from their Austrian colleagues to back up their argument. Dr Oder can refer to a study carried out at his hospital involving 700 patients who suffered no retrospective complications after percutaneous infiltration with crystalline corticosteroids.
Profile:
A Zurich University Hospital medical graduate, and from 1991-2001an employee at Vienna’s Medical University and the city’s General Hospital, and then Deputy Head of Interventional Radiology at the University Clinic for Radiodiagnostics, since 2002 Professor Siegfried Thurnher, EBIR, has led the Radiology and Nuclear Medicine Department at St. John of God Hospital in Vienna. The professor is an internationally sought after lecturer, having delivered around 200 at scientific congresses. He has also been a Live-Case Surgeon as well as moderator of numerous workshops.
03.03.2014