Article • Hybrid
The whole is greater than the sum of its parts
‘The combination of nuclear medicine and modern imaging procedures such as CT and MRI is becoming increasingly important in the diagnosis, treatment planning and aftercare of cancerous diseases,’ explains Professor Katrine Åhlström Riklund, who presides over the newly established European Society for Hybrid Medical Imaging, ESHI.
Report: Michael Krassnitzer

Hybrid Imaging was among the main topics at this year’s European Congress of Radiology (ECR 2016) in Vienna this March. Riklund, this year’s congress president, said, ‘The molecular, biochemical and structural information obtained through hybrid imaging is greater than the information gathered from the respective individual procedures.’ Or, as Aristotle put it: ‘The whole is greater than the sum of its parts’.
PET/CT, the combination of positron-emission-tomography and CT, and SPECT/CT, the combination of single photon emission CT and CT, are already fixed components of radiological and nuclear medical diagnosis. However, there are also new developments in this area of medicine.
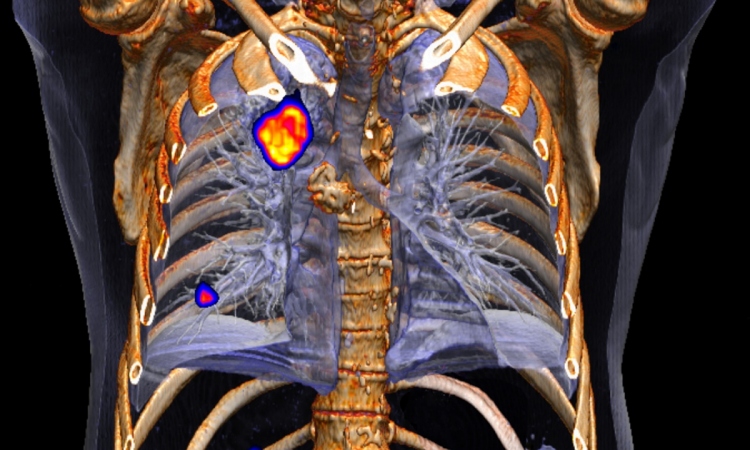
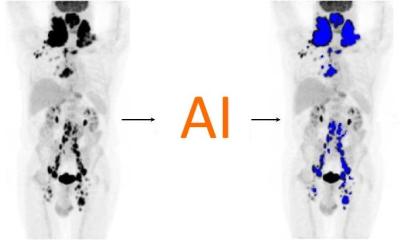
Researchers from the Statistical Imaging Group at University College Cork, Ireland, as well as researchers from the Department for Radiology and the PET/CT Unit at the University Hospital Cork, reported on statistical methods they have developed to analyse 18F-FDG-PET/CT examinations.
With the help of the tracer 18F-fludeoxyglucose a lot more information can be gained about heterogeneous tumours than with conventional PET/CT. Lung cancer for instance is characterised by a particularly high tumour heterogeneity, i.e. the tumours contain a number of genetically different cancer cells with different biological characteristics – a fact that must considered during treatment.
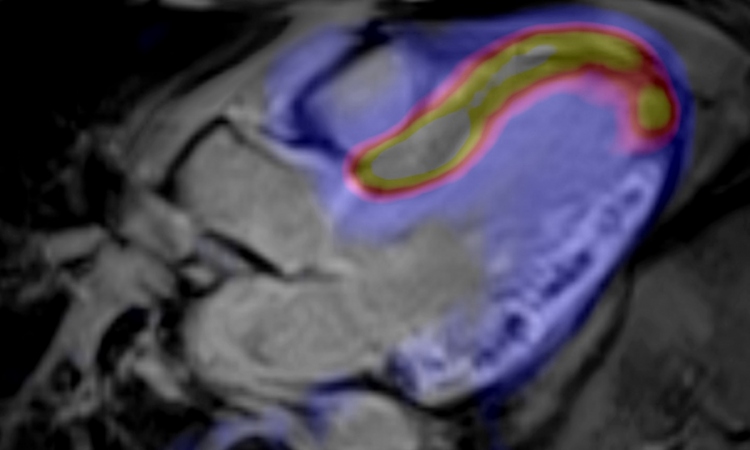
Even more is happening in PET/MRI, i.e. the combination of positron emission tomography and magnetic resonance tomography. "PET and MRI are still in their 'honeymoon period'," Professor Vivky Goh, Chair of Clinical Cancer Imaging at King’s College London, points out, although she can also see a shift in paradigm. ‘The times where we simply used to measure whether a tumour has grown or shrunk are over. Now we actually have access to the biology of the tumour.’
Professor Gary Cook, Chair of Clinical PET Imaging at King’s College London is somewhat less euphoric: ‘It’s not yet clear how important PET/MRI will become as a diagnostic tool.’ However, even he ultimately sees a rosy future for PET/MRI. ‘There is mounting evidence that PET/MRI delivers a more precise diagnosis for some types of tumours, such as those in the brain or prostate, than PET/CT or MRI alone.’ The use of new tracers, such as Gallium 68 (68Ga) could also give PET/MRI a boost.
As multiparametric MRI is acquiring a key role in the diagnosis of prostate cancer, now PET/MRI is also becoming of interest in this field. ‘Particularly in the case of recurrences, PET has proved to be a useful tool to differentiate between potentially curable local recurrences and metastases,’ explains Dr Egesta Lopci, from the Department for Nuclear Medicine at the Istituto Clinico Humanitas in Milan, Italy. Choline tracers (11 C-Choline and 18F-Choline) are used for this purpose. Prostate cancer cells have a high requirement for choline, which means that this respective radionuclide is found there in particularly high concentrations.
In the case of dementia, PET/MRI could also play a more important role in the future. Although MRI makes it possible to differentiate between the typical patterns in the brains of Alzheimer patients, and those suffering vascular dementia, this is only possible for the typical forms. ‘Individual patterns often don’t look like those found in textbooks and there are patients who suffer Alzheimer dementia as well as vascular dementia,’ explains Dr Sven Haller, neuroradiologist at the University Hospital Geneva, Switzerland. There is also the problem of the ‘blind spot’, which MRI is affected by during the detection of Lewy Body Dementia: ‘MRI is nonspecific when it comes to the detection of this type of dementia,’ he adds.
Thus PET comes into play: ‘This procedure makes it possible to determine the reduced dopamine transporter reception in the striate nucleus that occurs with Lewy Body Dementia. PET also facilitates a clear differentiation between Alzheimer dementia and vascular dementia. ‘The crucial point is the detection of beta-amyloid in vivo,’ emphasises Dr Valentina Garibotto, specialist in nuclear medicine at the University Hospital Geneva. There are no fewer than four tracers that can be utilised to detect typical plaques of beta-amyloid, which accumulate in the nerve cells and blood vessels of the brain in Alzheimer sufferers.


‘The availability of PET/MRI opens up new possibilities in oncological radiotherapy,’ confirms Professor Ursula Nestle, of the Department for Diagnostic and Therapeutic Radiology at the University Hospital Freiburg (Germany): ‘The hybrid procedure facilitates very precise therapy planning.’ This applies in particular to tumours which can only be visualised with difficulty with CT but very well visualised with MRI and which can also be examined very well with PET, such as those found in the upper abdomen, prostate and brain.’ Nestle is expecting a lot from the combination of molecular PET and molecular MRI.
Recently launched is a new EU breast cancer research project, ‘Digital Hybrid Breast PET/MRI for Enhanced Diagnosis of Breast Cancer’ (HYPMED). The European Institute for Biomedical Imaging Research (EIBR) runs this, as project coordinator, and the University Hospital Aachen, Germany is scientific coordinator. The project envisages the integration of a PET detector into an MRI surface coil so that high resolution PET imaging and high resolution MRI imaging can be carried out synchronously in breast cancer patients – including the opportunity to carry out minimally invasive MRI- and PET-guided biopsies. ‘This approach is basically aimed at upgrading any conventional MRI scanner into a high resolution PET/MRI system,’ confirms Professor Volkmar Schulz Dr-Ing, from the Institute for Experimental Molecular Imaging at University Hospital Aachen.
The growing importance of hybrid imaging also has an impact on the relationship between radiologists and nuclear medics. ‘This combination of nuclear medical and radiological procedures requires specialist knowledge of both disciplines and also respective training,’ emphasises Professor Osman Ratib, Head of the Department for Nuclear Medicine and Molecular Imaging at University Hospital Geneva.
However, this is not quite so easy: ‘Whilst hybrid imaging is developing at a rapid pace there is still room for improvement when it comes to the cooperation between both disciplines involved,’ believes Professor Gerald Antoch, Director of the Institute for Diagnostic and Interventional Radiology at the University Hospital Dusseldorf. Nuclear medics should not simply regard CT or MRI as tools for the precise anatomic positioning of their PET images, and radiologists should not only see PET and CT as types of additional contrast media, Antoch believes: ‘We need training programmes that cover both sides of hybrid imaging.’
ESHI president Riklund taps it in a nutshell: ‘In the future hybrid images should be interpreted by one single specialist.’
28.06.2016