The new world of biomarkers
Mark Nicholls reports
While biomarkers are acknowledged as useful tools in the early assessment of patient response to treatment, radiologists are less clear on how they can be applied in clinical practice. The ECR session Biomarkers: new word, new world, new work? explored a number of new applications for biomarkers with senior radiologists discussing their relevance in different areas.

Dr Anwar Padhani, consultant radiologist and head of imaging research at the Paul Strickland Scanner Centre, Mount Vernon Hospital, Northwood, London, who chaired the "Biomarkers: new word, new world, new work?" session, explained: ‘As radiologists, what we need to know is how useful biomarkers are to us as clinicians, what we think needs to be done in terms of making them useful and how we make the best use of them in terms of disease characterisation and for assessing drug responses.’
Biomarkers are an indicator of a biological state, but while radiologists have used anatomical imaging biomarkers in a ‘qualitative’ way to assess whether what is captured on the image is bigger or smaller, for example, ‘quantitative’ evaluations are viewed as the way of the future, in that they measure volumes, lengths, metabolic rates and blood flow.
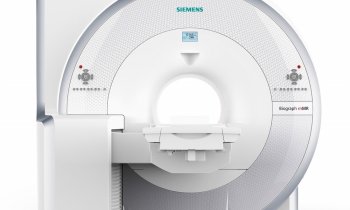
Dr Padhani added that the session’s objectives were to understand the challenges of clinical diagnosis and management and of drug development; to understand that cancers have unique hallmarks including cellular proliferation, tissue hypoxia, angiogenesis, many of which can be imaged and used for diagnosis, to assess therapy response and its outcome and for drug development; to review the biological basis and evidence for MRI and PET biomarkers that are ready for clinical translation; and to consider methods for predictive biomarker qualification. ‘It is a case of knowing what we can measure, how we measure and analyse it and how much progress is now needed to get it from a technique to something that is useful in a patient. For many radiologists, biomarker is a new word; a new world because they need to be aware that these techniques are emerging very rapidly.’
In effect, the session helped radiologists put biomarkers in a clinical context, help them begin to address the issues in clinical practice on a daily basis and bring a new dimension to the way they work in future.
The session had three other key speakers: Looking at what biomarkers are, Professor Bernard Van Beers, professor of radiology at Beaujon, Hospital, University of Paris-Diderot, France, will give examples of the major classes of biomarkers and how to distinguish biomarkers from surrogate markers. He will also explore what needs to be done for any biomarkers to be useful in the clinic and for drug development.
Professor David Lomas from the University of Cambridge, School of Clinical Medicine, will cite examples of MRI biomarkers that can be used to investigate abdominal disease, and Professor Eric Aboagye, Imperial College London, will talk about examples of PET tracers that can be used to investigate tumour biology.
The speakers enabled radiologists to get to know the clinical context, biological basis, measurement and analysis methods of biomarkers of angiogenesis, hypoxia and fibrosis and how to become familiar with the clinical evidence for biomarker, as well as look at the usage and limitations for each biomarker.
Looking at an illustrated framework for development of biomarkers, Dr Padhani focused on how dynamic MRI has progressed as a method for personalised assessment of therapy response in breast cancer. He also discussed whether imaging biomarkers can realistically be developed for their intended purpose and then chair a panel discussion on how radiologists could and should implement biomarkers in clinical practice.
06.03.2010