The MR-guided intra-operative surgical suite
Intra-operative MR imaging is still uncommon in Europe – particularly in neurosurgery. One of the first neurosurgery departments to work with a 3-T MR is in the Central Military Hospital in Prague. The experience and initial clinical findings from treating more than 300 patients, over a two-year period, was reported at this year’s ECR.

When EH correspondent Meike Lerner asked Dr David Netuka about the type of interventions performed in the hospital’s image-guided neurosurgery suite, he explained that there are two major areas in which his department mainly uses the intra-operative MR scanning option: pituitary adenomas and gliomas.
‘In the case of pituitary adenoma, we use all the modern technologies, such as endoscopy, but still cannot be 100% sure that we have removed everything. In that case, we stop the procedure, and transfer the patient from the operating theatre (OT) to the MR suite to perform intra-operative scanning. We then review the scans and decide whether we achieved our goal, or not. Is there a residuum that’s amenable for resection, or should we quit the procedure? Previously, you did the surgery without intra-operative scanning and waited three months for full MR scanning. With pituitary adenomas, it’s quite tricky to do MR scanning one day after surgery because of the possibility of haematoma and postoperative changes. We do it nowadays, but in the neurosurgical literature, the value of early postoperative MR scanning is questionable.’
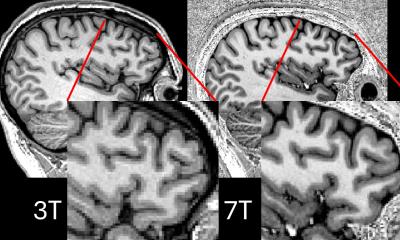
In April 2008, GE Healthcare’s 3.0-Tesla and 1.5-T Magnetic Resonance Neurological Suite was integrated into an operating theatre at the hospital. This uses 3-D imaging to navigate and validate treatments, helping to help increase the accuracy and speed of interventions and improve patient outcomes. ‘Since then,’ Dr Netuka said, ‘we’ve been able to increase the number of radical resections by 20 % in a group of 150 of those 300 patients. And we got the results that this increase was not connected with an increase of morbidity. If you are more aggressive in surgery, you could increase the morbidity but this was not the case.
‘For the glioma patients, not only the extent of resection can be enhanced, but we also try to decrease surgical morbidity by using functional images and tractographies. Here, we observed less second stage surgeries.’
Along with better patient outcomes, workflow has improved. ‘The MR suite is next to our operating theatre, so we only open the door and the surgical table is moved to the MR suite where we slide the patient into the MR scanner. Together with the neuroradiologist we discuss the cases we want to do in the OT, and then we select the sequences we want to do intra-operatively. It takes 12-15 minutes and everything is much faster; it works smoothly. But the crucial point is the cooperation between the neurosurgeon and the neuroradiologist.
Another important point: There are always concerns that if you do intra-operative scanning, and move the patient into another room, there may be an increased risk of infection. We can show there has been no increased risk of infections due to intra-operative scanning.’
Asked about other fields in which this practice could be of value, Dr Netuka said: ‘A quite innovative approach is its use for spinal cord tumours. Another interesting field is intra-operative tractography. The other point is intra-operative spectroscopy -- detection of a tumour remnant with a different imaging modality – which may be useful in the future.’
21.05.2010