Article • Clinical benefit
The future of telemonitoring
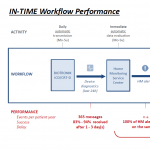
The IN-TIME study remains the only major trial to show a clear mortality benefit for remote monitoring in heart failure (HF) patients. A recent analysis by Hussar et al. suggests workflow processes such as daily, multiparametric data transmitted using Biotronik Home Monitoring, may be key to this benefit. Dr Wilfried Mullens, Head of the Heart Failure and Cardiac Rehabilitation Section at Ziekenhuis Oost-Limburg, in Genk, Belgium looks at the implications for telemonitoring in the future.
According to the recent Hussar et al. analysis, workflow processes might make a clear difference in remote monitoring’s clinical benefit. How should we now look at the IN-TIME?
Wilfried Mullens: ‘IN-TIME is a great study, but you have to incorporate it into a disease management strategy. Telemonitoring is a great tool if you know how to use it within a daily work schedule. If the study showed something, it was that when you react to telemonitoring signals in an appropriate and individualised manner, it can be beneficial.
‘There’s a lot of technical signals coming out of devices that don’t lead to a lot of clinical benefit. You need someone to filter those before they reach the physician or healthcare professional. You have to get to know your patient as well because some alarms will be important for some patients but not for others.’
How is an efficient remote monitoring workflow managed in your practice?
‘We’ve installed mandatory phone calls for certain alerts. In these phone calls, the nurses ask patients specific questions. Our EP nurses, who are absolutely fantastic, will sometimes say everything is fine. My heart failure nurse might call later for the same alert and be able to tell whether something’s wrong.
‘If you keep a direct link to that patient, you can then reinforce better adherence to medical therapy, for example. Telemonitoring can be a challenge in a lot of hospitals because it can take a lot of time to process technical alerts. We would look to manufacturers to make that more efficient.
‘At hospitals, we need to improve the way we look at data, by training two types of nurses—those who handle device problems and those who specialise in heart failure.’
Recommended article
Sponsored • Remote monitoring
It’s time to look again at IN-TIME
As the world’s largest cardiology congress gets underway in Munich, it’s worth looking back to previous ESC sessions to see how scientific debates have evolved. At ESC 2016, held in Rome, REM-HF investigators presented data suggesting remote monitoring in implantable cardiac devices offered no added clinical benefit. Two years on, there are new reasons to re-examine that conclusion, with a…
For telemonitoring, what should the next step be?
‘I think telemonitoring is here to stay and it’s going to expand. I think patients want some kind of self-empowerment and we’re almost there. For example, if I had paroxysmal atrial fibrillation only once every three months and I have an implantable device, why do I have to take anti-coagulants all the time?
‘If I see an alert on my phone saying I have to take an action to avoid a thrombolytic event, that would be a step forward.
‘The second thing is to train nurses to see what’s important in telemonitoring and to act on that information as independently of the physician as possible.'
Profile:
Dr Wilfried Mullens heads the Heart Failure and Cardiac Rehabilitation Section at Ziekenhuis Oost-Limburg, in Genk, Belgium.
22.10.2018





