The complex science behind microbubbles
At Bracco Suisse SA in Geneva all efforts are dedicated to contrast media for ultrasound scans. During their visit to the firm’s research centre and manufacturing site, Daniela Zimmermann and Ralf Mateblowski met with François Tranquart MD PhD, general manager of the Bracco Suisse research centre, to hear why SonoVue is now Europe’s most popular ultrasound contrast agent, with research heading towards novel agents aimed at detecting and imaging specific molecules that are key targets in disease processes (molecular imaging).
Microbubbles are highly complex and effective. Basically, François Tranquart explains, the ultrasound contrast agent SonoVue is formulated with microscopic microbubbles, smaller than red blood cells, and a non-toxic gas – sulphur hexafluoride. SF6 has low water solubility to prevent diffusion into surrounding blood and it is fully exhaled via the lungs within minutes. Microbubbles can be injected repeatedly in patients for better characterisation or treatment guidance. The microbubble shell is highly flexible and made of phospholipids, like the membranes of natural cells.
Bubble size is vital, since they must quickly flow through capillaries. The type of gas is the most important component of the microbubble, he explains. ‘There is a degree of diffusion between the microbubble core and surrounding environment – blood. A gas such as SF6 is not normally present in blood. It slowly diffuses from the inside towards the outside. With air, oxygen and nitrogen, however, there is a constant exchange of gas between bubbles and blood: the microbubbles would disappear right after injection. SF6 guarantees the microbubbles to last a few minutes, enough to make a diagnosis.
‘Obviously, we also want to improve the shell properties to protect microbubbles and make them more resistant to pressure because, once injected, they circulate in the blood and are exposed to ventricle contraction. Even with excessive hydrostatic pressure, they must persist. In general each microbubble has its own properties. Some are soft and may present different behaviours when exposed to different acoustic pressures. Others are a bit more resilient and thus less sensitive to acoustic pressure such as ultrasound waves. We need to play with different properties depending on selected indications.
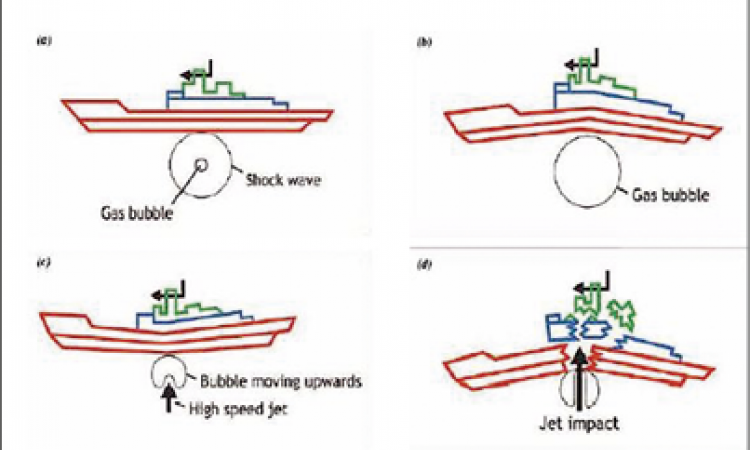
‘Ultrasound waves exert positive and negative pressures. We saw that soft shell bubbles respond sensitively to these acoustic waves when we matched the machine settings and microbubbles perfectly. Since this technology is complex we need to attune microbubble characteristics and the acoustic parameters of the equipment. If there’s a good match between microbubble properties and the ultrasound equipment, we obtain a strong and easily visible signal from these microbubbles to acoustic waves, so we could detect minute amounts of them in vessels and parenchymal organs using very small contrast agent doses. We can observe the specific behaviour of microbubbles expanding and shrinking depending on the acoustic waves. Under positive acoustic pressure they shrink, but with negative pressure, microbubbles expand.
By playing with these two different responses we detected a specific ultrasound signal, representing the presence of microbubbles with- in the bloods without overlapping tissue signal.
‘Ultrasound frequencies are relatively high and changes in acoustic pressures are very rapid. Under ultrasound all the microbubbles are oscillating around their stable state. This oscillation is the signal we detect. Its strength is proportional to the amount of microbubbles in the different areas. If we inject microbubbles they circulate and accumulate in some specific areas. By observing arrival, disappearance and persistence, we get important diagnostic information.
‘We can diagnose a tumour or inflammation based on the behaviour of the agent within the specific area because we know that a cancer lesion will exhibit a specific behaviour compared to an inflammatory lesion or normal tissue. When you compare a lesion with normal parenchyma, or an inflammatory lesion with a cancer lesion you will observe differences regarding arrival time, enhancement, or washout.’
‘In Europe, SonoVue is approved for use in echocardiography, Doppler sonography of large vessels and liver and breast lesions. Clinical trials demonstrated that ultrasound with this agent provides more diagnostic information than non-enhanced ultrasound in specific clinical settings.
Targeted microbubbles – the Ferrari in the Bracco garage
While SonoVue as a non-targeted agent reflecting blood flow and perfusion is state-of-the-art technology, the Bracco team is already highly engaged developing a new generation of microbubbles, ‘targeted agents’ as François Tranquart explains: a specific ligand placed on the shell so the microbubble can bind a specific receptor.
‘When it comes to detection and characterisation of focal parenchymal lesions, with SonoVue we can tell where a lesions is, if such lesion is highly or poorly vascularised, and the type of enhancement (wash-in, peak, wash-out) can give us clues about its nature’ he points out. ‘With targeted microbubbles, on the other hand, we are moving into molecular imaging: the ligands bind specific receptors expressed by cells. Thus, we can image molecular patterns in some specific regions of the living body, comparable to immunohistochemistry used by the pathologist in biopsy specimens. The aim is to see exactly what is expressed and the level of expression in a living body. The presence of a specific receptor or specific protein could explain if and how disease processes are taking place. That means, firstly the information gathered with the targeted agent is much more specific. Secondly, in the future we may be able to monitor treatment efficacy in a different way, because some treatments could interact with this receptor changing its expression, which we could directly image.’
‘We need to target receptors expressed within the vessels. Since the microbubbles remain strictly within the vessels we cannot target receptors expressed in tissues. This is a key point. As many diseases are associated with specific receptors, we have to select relevant receptors expressed on endothelial cells. This is the case for many receptors involved in the angiogenesis process where they are expressed at endothelial level and require a specific ligand (such as VEGF, HIF and many others) to induce angiogenesis. The aim of targeted bubbles is to use this process with a ligand which is close to the natural one.’
If these could detect angiogenesis, might suppression be a next step?
‘Theoretically speaking, maybe; practically speaking, I don’t think so. We have very few attached microbubbles but a huge number of receptors, which makes blocking the physiological process impossible. Besides, microbubbles disappear in minutes. However, demonstrating the presence of a specific receptor involved in the disease process might lead to treatment specifically directed towards such a target. If, for example, dealing with a local angiogenesis then having that ability would provide a clear indication that an anti-angiogenic treatment is effective in eliminating the blood supply to cancer cells. Such an approach, where medication is adjusted to the specific situation of the individual patient, is “precision medicine”.’
What about a new generation?
‘After identification and labelling of pathological tissue, a third generation could even guide drugs to a specific site.’
29.10.2013