Article • ECR Round table discussion
Specialists build bridges in interventional oncology
Delivering a drug directly inside a lesion using minimally invasive procedures opens up new perspectives for patients and medical teams. At the ECR Overture, speakers looked at how to best join forces to advance the promising field of interventional oncology during a round table discussion.
Report: Mélisande Rouger

Injecting a chemotherapeutic agent into a tumour locally has gained ground in clinical practice, but there is still some way to go before immunotherapy or other target agents are used in this setting, according to Prof Dr Thomas Helmberger. The Chairman of the Department of Radiology, Neuroradiology, and Minimally Invasive Therapy at Munich Klinik Bogenhausen, Germany, made a case for more interdisciplinarity as he opened the session: ‘I’ve been lucky to work closely with oncologists and surgeons for many years,’ he said. ‘Traditionally, specialists dealing with oncological patients tend to stick to their specific therapies for a long time before they even consider trying something else. Nevertheless, joining efforts for our patients will be worthwhile.’
Stepping out of the comfort zone
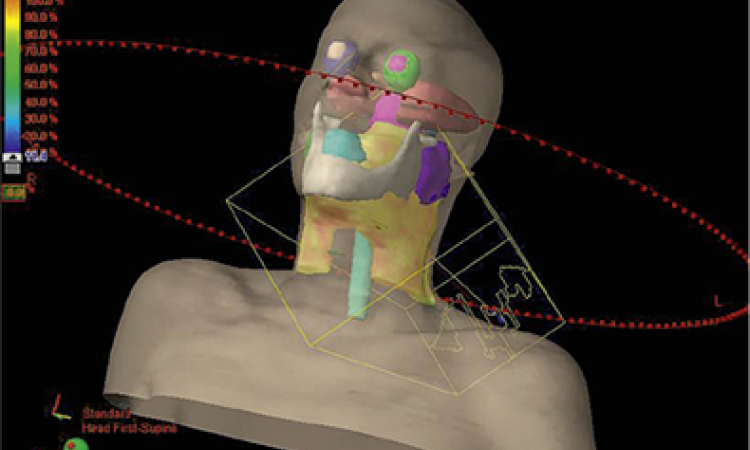
While he sympathised with oncologists being cautious about interventional oncological treatment options, or even feeling “threatened” by interventional radiology, Helmberger advocated that they should not hesitate to seek radiologists’ support to provide collaborative therapy concepts. ‘Interventional oncology has proved its efficiency and safety in hundreds of thousands of patients worldwide. When the first procedures were introduced 30 years ago, other specialties were sceptical too. Now, tumour embolisation for hepatocellular cancer, radioembolisation and thermal ablation – to name a few – are standard,’ he said.
Interventional oncology is much more interactive and challenging for radiologists because they have to think like an oncologist and learn about new terminology
Thomas Helmberger
Today, peripheral and cerebral vascular procedures remain at the core of interventional radiology’s scope. One of the main obstacles to further deployment in oncology is the reluctance of many radiologists to work in this setting since it might be more demanding. ‘Interventional oncology is much more interactive and challenging for radiologists because they have to think like an oncologist and learn about new terminology,’ Prof Helmberger said. ‘They have to deal with patients who are often much sicker, facing complex therapies, and they also have to advise their families, just like a surgeon or an oncologist would.’
An aging population and increasing cost pressure on healthcare systems accelerate the trend for hospitals to deliver smart multimodality treatment options, the expert predicted. In this setting, radiologists can provide more than just reading scans. ‘You’ll have to learn to leave your comfort zone and step into the treatment field,’ he said, addressing his radiologist colleagues. ‘Interventional oncology is a very smart career choice for the new generation.’
Clear benefits for the patient
The expert went into detail on the benefits of interventional oncology, which can help oncologists manage systemic treatments’ side effects in patients. For instance, local application of low dose chemo or immunotherapeutic agents can also allow disease control, while significantly reducing side effects in patients with localised tumours in the lung or kidney.
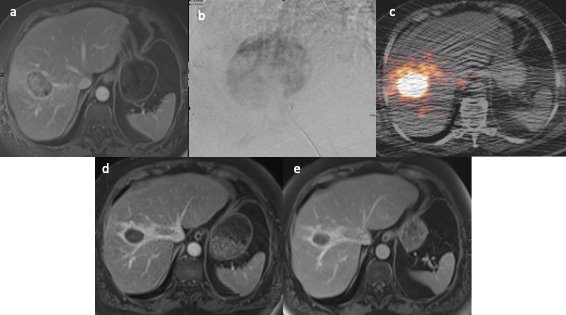
Prof Helmberger reported on how he often carries out liver focused therapy such as chemoembolisation not just in hepatocellular cancer, but also metastatic disease of colorectal cancer, to help patients recuperate between chemo or immunotherapy cycles. ‘Offering patients a pause helps them to recover. During this break, oncologists may also decide whether further treatment is necessary or not, if they see that their patients are getting better,’ he said.
Triggering a chain reaction

Directly delivering treatment inside a tumour (intratumoral therapy) may have an impact not only in the lesion itself, but also on other tumour locations in the body, Prof Dr Andrés Cervantes, Head of the Medical Oncology Department at the University Hospital of Valencia, Spain, explained in the following talk. ‘For example, if you inject a drug in a 2cm nodule of a given compound in the liver, you may also get a response in a cervical node. This reaction also applies to other parts of the body.’ Thus, the goal is to use this treatment effect in a specific accessible lesion to combat additional cancers. ‘The only requirement is that the tumour is at least 2cm in size and can be injected without the risk of a toxic event,’ he said.
Intratumoral immunotherapy is a strong area of development now; researchers are looking into what agents or drugs may stimulate the immune response more effectively when injected into a given tumour. Some of the trials are exploring the efficiency of existing anti-cancer drugs that have not been FDA-approved in that context yet. ‘We have huge preclinical evidence that this could be a very important finding, but it’s still very early and we have to consider safety and toxicity issues,’ said Cervantes.
Together with his multidisciplinary team at INCLIVA Institute of Health Research, the expert is working on advancing this approach. ‘Radiologists need us because we have patients and we need them because they have the techniques and tools that may improve patients’ outcomes and help surgery develop further,’ he concluded.
In another talk, Dr Guido Torzilli, Head of the Liver Surgery Department at the Humanitas Research Hospital in Milan, Italy, explained how surgical oncology is moving towards minimally invasive treatments for the patient’s benefit.
Profiles:
Thomas Helmberger is Professor of Radiology and Chairman of the Department of Radiology, Neuroradiology, and Minimally Invasive Therapy at Munich clinic Bogenhausen, Germany. His medical specialties include diagnostic imaging of the abdominal and thoracic organs, including functional and tissue-specific imaging (liver, pancreas, small and large intestine), the spectrum of diagnostic and interventional vascular medicine, and interventional oncology.
Andrés Cervantes is Head of the Medical Oncology Department at the University Hospital of Valencia and Professor of Medicine at the University of Valencia, Spain. He is the General and Scientific Director of the Institute of Health Research - INCLIVA. His main areas of interest and research are gastrointestinal and gynaecological cancer, as well as Phase I trials and new drugs development.
11.04.2022