Smell
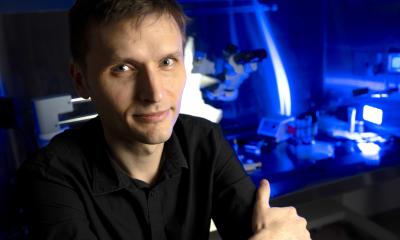
By Professor Thomas Hummel, of the Smell and Taste Clinic, Department of Otolaryngology, University of Dresden Medical School, Germany
The sense of smell exhibits numerous peculiarities. Odorous sensations, and most importantly, flavours, are typically not only brought about by the olfactory system, but other sensory channels are also involved in this chemosensory perception, namely the gustatory system, mediating sensations like sweet, sour, salty, bitter, and umami, or the trigeminal system mediating sensations like tickling, tingling, stinging, or burning. Thus, smells or, even more so, flavours are the result of the integration of sensory information through many different channels.
Humans express approximately 350 olfactory receptors. Every olfactory receptor neuron only expresses one single olfactory receptor gene. Further, axons from all olfactory receptor neurons expressing the same olfactory receptor project to two specific glomeruli in each olfactory bulb. This organisation is called glomerular convergence. Olfactory receptors are not selective for only one odorant but numerous molecules may bind with varying affinities to a certain olfactory receptor. Thus, odorants are typically not only recognised by one but by several olfactory receptors simultaneously, according to their particular chemical properties. At the level of the olfactory bulb this leads to a specific activation pattern for each odorant, which is believed to be responsible for the discrimination between different odorants.
Other than other sensory systems the majority of the olfactory fibres does not cross to the contralateral hemisphere but projects ipsilaterally to the brain. Second, most olfactory fibres bypass the thalamus and project very early and directly to the pyriform cortex, amygdalae, and entorhinal cortex, which are implicated in emotional and memory processing. This particular anatomy is claimed to be responsible for the emotions and memories produced by many odours. In addition, the olfactory system exhibits amazing plasticity on several levels: On the level of the epithelium, olfactory receptor neurons are continuously replaced throughout lifetime. Similarly, on the level of the olfactory bulb interneurons are being replaced constantly (accordingly, the volume of the olfactory bulb decreases in cases where sensory input to the bulb is lost, e.g. following head trauma with severed fila olfactoria). Such plasticity provides a basis for adaptive capabilities of this system, which allows humans to adjust quickly to environmental challenges. It is also the basis for recovery of olfactory function following destruction of olfactory receptor neurons, e.g., following infections of the upper respiratory tract.
In a clinical context testing of olfactory function is important as many people misjudge their olfactory capabilities. To this end, standardised systems are readily available, e.g. the Sniffin’ Sticks. Apart from simple, but effective screening test, these test kits contain subtests for odour identification, odour discrimination, and odour thresholds. In addition, electrophysiological techniques like olfactory event-related potentials allow to objectively measure whether subjects perceive an odour or not. Such techniques are important when it comes to the diagnosis of olfactory loss - which is not a rare finding. In fact, 5% of the population are anosmic! The highest incidence of olfactory loss is found in the age group above 65 years, indicating that we typically lose olfactory abilities as we age.
Accordingly, the quality of our lives decreases as we age, especially because we are less able to enjoy sophisticated (or not so sophisticated, but delicious) foods and drinks. In addition, people with loss of olfactory function experience hazardous situations like eating spoiled foods or not recognising smoke or gas leaks.
Apart from ‘aging’ as a significant cause of olfactory loss, there are four other major causes: (1) sinunasal disease, e.g., chronic sinusitis or nasal polyposis, produces a gradual decrease of olfactory function; (2) olfactory loss is found after head trauma, and here particularly frequent after occipital trauma; (3) infections of the upper respiratory airways, e.g. a cold or a flu, and (4) neurodegenerative disease like Alzheimer’s disease of Parkinson’s disease. Interestingly, olfactory loss is an early sign of Parkinson’s disease preceding motor symptoms by several years. This symptom is so reliable that in patients with signs of Parkinson’s disease but normal olfactory function the diagnosis should be revisited.
With regard to therapy, relatively little can be done in patients with olfactory loss. Patients with sinunasal disease can be treated through surgical or anti-inflammatory regimens using both systemic and local corticosteroids. In patients with post-traumatic or post-infectious olfactory loss so far no conservative treatment has been established. However, recent studies show that training of the sense of smell (the rigorous practice of daily sniffing of four odours in the morning and evening over a period of 4-6 months) is beneficial to patients with olfactory loss. In addition, approximately 40-60% of patients with post-infectious olfactory loss and 10-20% or patients with post-traumatic olfactory loss experience recovery of the sense of smell over a period of 1-3 years. Considering the therapeutic void it appears important to counsel patients with regard to their
prognosis.
02.08.2006