Article • Men are from Mars, women are from Venus
Sex differences in imaging cardiovascular disease
An interplanetary title for a quite down-to-earth topic: The symposium "Men are from Mars, women are from Venus" at the EACVI congress (European Association of Cardiovascular imaging) launched into the differences between the hearts of men and women.
Article: Wolfgang Behrends
Image credit: G.Hüdepohl (atacamaphoto.com)/ESO (CC BY 4.0)

Image source: ACC/ESC
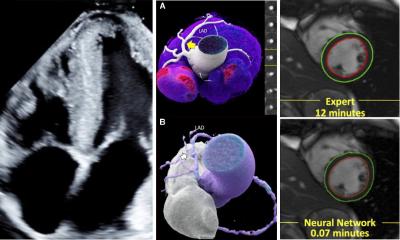
While the speakers could firmly establish that both sexes share the same home world, variations in their cardiac anatomy warrant a more gender-specific approach to imaging. To this end, Patricia Ann Pellikka, MD, Professor of Cardiovascular Disease Clinical Research at Mayo Clinic in Rochester, Minnesota, went into detail on how aortic valve disease presents differently in male and female patients, and why current guidelines put women at a clear disadvantage.
The session title references John Gray’s relationship guide, but for Dr Pellikka, the distinctions between men and women run deeper than the psychological level: ‘There are anatomic, physiologic and pathophysiologic differences between the sexes that have implications for aortic valve disease, and for our role as imagers.’
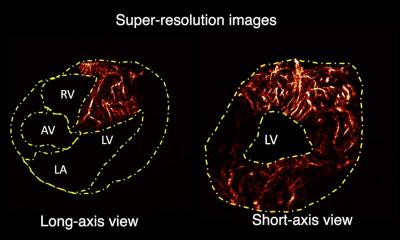
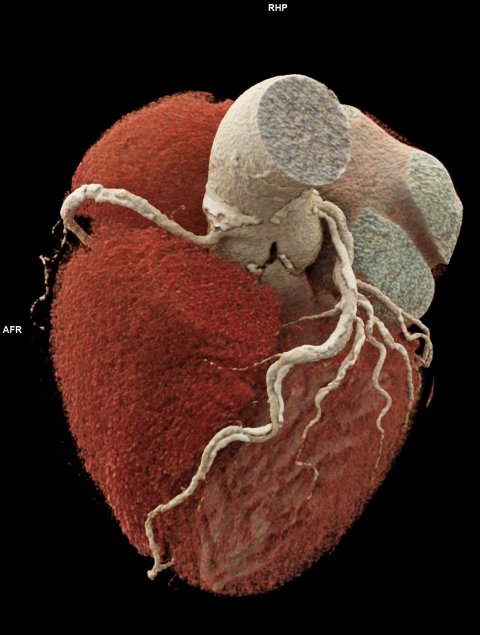
For one, stenotic valve leaflets in women tend to have less calcification, but a higher degree of fibrosis than men. Their aortic annulus is smaller, and their coronary height is lower.1 ‘Of course, this has implications for aortic valve prosthetic sizing,’ the expert pointed out. ‘And, in the way of left ventricular remodeling, women are more apt to have hypertrophy that results in a narrowing of their left ventricular cavity, as opposed to eccentric hypertrophy, which is more prevalent in men in aortic stenosis. Women also have more extracellular matrix and more myocytes will be found in men.’
There is something about women that prevents their aorta from dilating, presumably due to differences in the aortic wall
Patricia Ann Pellikka
But how do these changes affect disease progression? ‘Many studies have suggested that progression of aortic stenosis is similar in men and women, but a couple of recent CT studies suggest that once calcification is present, it may actually progress more rapidly in women.’2 In higher age groups, the imbalance becomes even more pronounced: while for patients over 65, the ratio of men to women with aortic stenosis is already at 1 : 1,25, in the 85+ age group, it rises to 1 : 1,78.3 This imbalance can also work the other way around, for example with biscuspid aortic valve (BAV), a disease that affects men more than twice as often than women.4
In addition to differences in prevalence of such conditions, symptoms may also differ between the sexes, the expert stated. As BAV patients, men typically present with aortic regurgitation, aortopathy, aortic dissection or endocarditis, while women are more often affected by aortic stenosis. ‘There is something about women that prevents their aorta from dilating, presumably due to differences in the aortic wall.’ This is also reflected in altered hemodynamics, where women with severe aortic stenosis tend to have lower stroke volume, peak velocity, and aortic valve area, but higher left ventricular filling pressure and E/e’ ratio.5
Guidelines geared towards male hearts
However, current guidelines for valvular heart disease largely fail to factor in these differences, resulting in women falling through the diagnostic cracks, Dr Pellikka warned: ‘These guidelines emphasize the importance of peak velocity and mean systolic gradient in characterizing severe aortic stenosis. I think the valve area is something we need to particularly pay attention to in women. Because of their lower stroke volume, they may not achieve the same gradient and peak velocity as men, even for severe aortic stenosis.’
© Universitätsklinikum Freiburg
Timing of intervention in chronic aortic stenosis currently depends on when a patient becomes symptomatic or presents with a high left ventricular end-systolic dimension (LVESD) – both parameters work against female cardiac characteristics: ‘When we wait for the patient to be symptomatic, we may be waiting too long,’ the expert said. ‘In asymptomatic patients, if we fail to index for body surface area, women will tend to not qualify for surgery.’
This puts female patients at a serious disadvantage, as aortic valve surgical intervention (AVS) significantly improves survival in patients with chronic aortic regurgitation (AR).6 ‘Women have a survival disadvantage in chronic AR – but if they do make it to surgery, they do just as well as men.’
Summarizing her presentation, Dr Pellikka urged her audience to be aware of the sex differences in heart anatomy and pathophysiology in women, which may impact progression of aortic valve disease and lead to undertreatment of female patients. ‘As imagers, we need to remember to index the left ventricular size, using either volumes or linear dimensions in aortic regurgitation,’ she added. ‘In aortic stenosis, remember to look carefully at the aortic valve area, not just the peak velocity and mean gradient. Consider CT calcium scoring if the aortic stenosis severity is uncertain.’
Following up on the presentation, the EACVI session learned about sex differences in mitral valve disease – as explained by Hector I. Michelena, MD, – as well as in atherosclerosis – presented by Leslee J. Shaw, PhD, – and their respective impact on imaging.
Profile:
Patricia Ann Pellikka, MD, is Professor of Cardiovascular Disease Clinical Research at Mayo Clinic in Rochester, Minnesota, USA. Her professional interests include echocardiography, artificial intelligence, imaging, and stress testing, and their application to valvular heart disease, heart failure, carcinoid heart disease, and ischemic heart disease. She is Editor-in-Chief at the Journal of the American Society of Echocardiography and has contributed – often as first author – to numerous publications concerning the non-invasive detection of cardiovascular disease and timing of intervention.
References:
- Shan Y, Pellika PA: Aortic stenosis in women; Heart 2020
- Nguyen V et al.: Sex Differences in the Progression of Aortic Stenosis and Prognostic Implication: The COFRASA-GENERAC Study; JACC: Cardiovascular Imaging 2016
- Eveborn GW et al.: The evolving epidemiology of valvular aortic stenosis. the Tromsø study; Heart 2013
- Kong W et al.: Bicuspid Aortic Valve: What to Image in Patients Considered for Transcatheter Aortic Valve Replacement?; Circulation: Cardiovascular Imaging 2017
- Ito S et al.: Sex Differences in LV Remodeling and Hemodynamics in Aortic Stenosis: Sex-Specific Criteria for Severe Stenosis?; JACC: Cardiovascular Imaging 2022
- Yang L et al.: Sex Differences in Outcomes of Patients With Chronic Aortic Regurgitation: Closing the Mortality Gap; Mayo Clinic Proceedings 2021
22.01.2024