Seeking congenital cardiac defects
Congenital heart defects are the most common congenital disorders found in newborns – around one in a hundred babies are affected. This type of heart defect can be reliably diagnosed with ultrasound, usually during the detailed foetal scan carried out halfway through the pregnancy.
Report: Brigitte Dinkloh


Congenital heart defects are the most common congenital disorders found in newborns – around one in a hundred babies are affected. This type of heart defect can be reliably diagnosed with ultrasound, usually during the detailed foetal scancarried out halfway through the pregnancy.
‘Experts can rule out up to 90% of heart defects prenatally,’explains gynaecologist Dr Kai-Sven Heling, who runs a practice for prenatal diagnostics in Berlin-Mitte.Heart with colleague Professor Rabih Chaoui. ‘Defects can be detected from the first trimester during nuchal translucency screening, particularly in cases involving a missing heart ventricle or valve. However, ventricular septal defects can only be accurately diagnosed from the 22nd week of pregnancy,’
Common heart defects
Before birth, heart defects are not normally relevant; they only become critical once the child’s circulation has to work independently. Generally, the more defects there are, the worse the prognosis for the baby. Therefore, timely diagnosis has a crucial impact on the chances of survival because it prevents discharge as supposedly healthy and then the baby develops problems at home. ‘This can easily be avoided because, as soon as the diagnosis is clear, we can increase the baby’s chances of survival, by inducing the birth in a specialist clinic, for instance.’
Ventricular septal defects (VSD), also known as a ‘hole in the heart’ and which cannot be completely ruled out prior to birth, are among those that patients can grow out of; indeed, in some cases the holes are so small that they are not necessarily visible, and sometimes they grow together again spontaneously. A hole between the two atria is also not necessarily a pathological diagnosis, as this will only close up after birth. Only when this hole doesn’t close in the postnatal phase can a heart defect be diagnosed.
‘A stenosis of the pulmonary artery is a much more common defect seen after birth than we see prenatally,’ Dr Heling pointed out. ‘We quite often misdiagnose this and, even when there is a diagnosis, we don’t always treat this defect, despite the fact that the children sometimes have clinical symptoms and turn blue under stress. Yet, sometimes children also grow out of this problem without the development of any noticeable, clinical symptoms.’
Surgery for heart defects
Immediate intervention after birth is essential for a number of cardiac defects, particularly where no, or clearly too little, blood flows into the lungs, i.e. where the child has no oxygen supply. This is normally the case with transposition – a reversal of the great arteries. Prenatal intervention is still an experimental concept here and not yet a gold standard of medicine. This procedure is currently being controversially discussed, with the largest expertise in this field within Europe, found at the Linz centre.
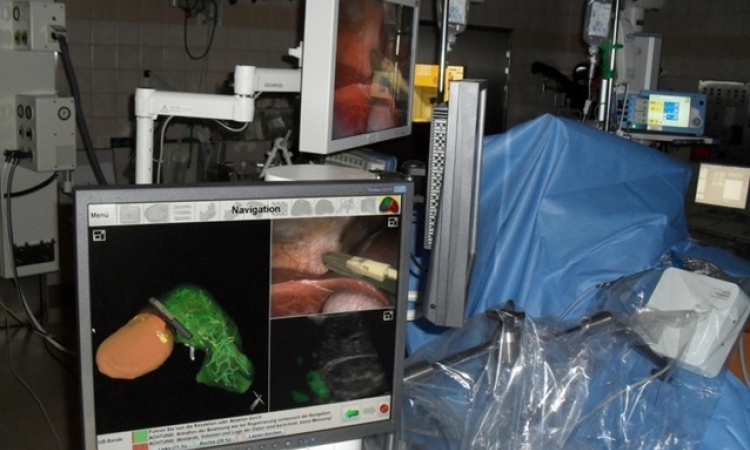
Prenatal interventions are particularly relevant when the aorta is too narrow and the left ventricle cannot develop correctly. If this occurs, in the long term it can lead to a lack of left ventricle functionality and eventually to single-ventricle circulation. ‘To avoid this, the valve is opened with the help of a catheter. However, this only helps to restore normal cardiac function with two working ventricles in a third of cases. In any case, only a small group of patients can be considered for this type of intervention because the prenatal, high-risk operation can only be considered before the ventricle loses functionality.’
The three-step Norwood procedure is more promising. After birth, the circulation is initially maintained with the help of medication to counteract the impaired left ventricular function, so that these newborns do not develop clinical symptoms. In the next step, an intervention is carried out to switch the arteries to ensure that a sufficient amount of blood flows into the circulation from the right ventricle. This is followed by more surgery after three months and then after three years. The child still only has a right ventricle, with the blood being passively passed into the lungs.
As yet there are no conclusive evaluations to confirm how promising the Norwood procedure is; however, reports suggest that the problems are merely delayed from childhood into adulthood.
‘There are heart defects that can definitely be corrected,’ Dr Heling said. ‘Therefore, from our point of view, it’s therefore tragic when these children still die nowadays because the defects were not detected during a detailed diagnosis. There are other heart defects that are now operable but which entail a life with limitations for the patients.
‘Nevertheless, this must still be considered positively and the patients do benefit from the fact that the defects can be diagnosed prior to birth, so they can be operated on in a stable condition.’
Therefore, Heling sums up, ‘…it’s important to be self-critical with one’s own diagnoses and to utilise the technology in the best possible way. An ultrasound image is only ever as good as the examiner and what he or she concludes, or suspects respectively.’
Profile:
Following medical studies at Humboldt University, Berlin, Kai-Sven Heling MD trained as a specialist at the University Women’s Clinic Charité, where then became a consultant there. The subject of his doctoral thesis was the foetal heart. Since 2005, he has worked in his own surgery, the Friedrichstrasse Practice, in Berlin. He also manages the Gynaecology/Obstetrics section at the German Society of Ultrasound in Medicine (DEGUM) and holds a Level III DEGUM qualification.
11.11.2014