Image source: LUMC
News • Vascular and Neurosurgery
New procedure to prevent phantom pain after limb amputation
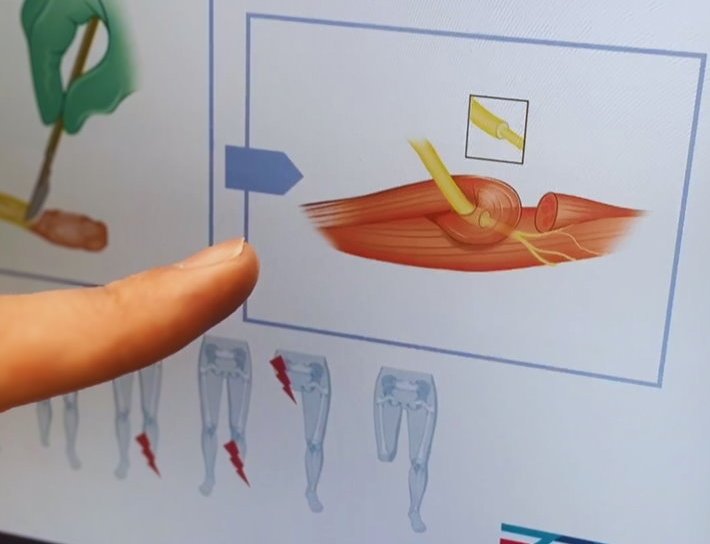
In the Netherlands, around 3,300 leg amputations are performed annually. Currently, the standard procedure is for a surgeon to tie off or burn the ends of the severed nerves, which leaves nerve damage in the stump.
In more than half of the cases, this leads to post-amputation pain such as phantom pain, the pain felt in an amputated limb. This pain can severely impact a person’s daily functioning and lead to high medication use.
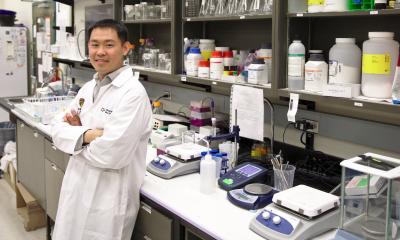
Each nerve has a regenerative ability, the ability to heal itself. A severed nerve will therefore grow out, seeking to connect with the rest of the nervous system. This nerve scar can cause a lot of pain. "Neatly cutting and storing it can help, but even better is to give the nerve something to do," says Justus Groen, neurosurgeon at the Leiden University Medical Center (LUMC). "In this case, we do this by attaching the severed nerve to the nerve ending of a muscle in the stump. Because the nerve has a connection again, it will not form a painful nerve scar. That is the biggest gain. The result is that people can start mobilizing after the amputation and, for example, wear a prosthesis."
I know the technique, but it’s like setting up a camping tent: in practice it can be slightly different. You need to have done it a few times to get it exactly right
Jan van Schaik
The technique described by Groen is not new. In practice, it has already been shown that the method works. However, this procedure is usually performed only after a patient has developed post-amputation pain, often weeks or months after the amputation itself. The downside is that the patient has to undergo surgery again.
The LUMC and six other Dutch hospitals want to perform the nerve surgery preventively, at the time when the leg is being amputated and the patient is still on the operating table. To provide definitive scientific proof that the method works, the involved centers, led by the LUMC, will start a study this summer. Doctors estimate that the nerve surgery will only add half an hour to the operation time.
For the study, nerve surgeons and vascular surgeons at the LUMC will work closely together. Initially, the vascular surgeon will perform the amputation and the neurosurgeon will connect the nerve. Later, the aim is for vascular surgeons to also perform the nerve procedure. Vascular surgeon Jan van Schaik: "I know the technique, but it’s like setting up a camping tent: in practice it can be slightly different. You need to have done it a few times to get it exactly right. That’s why we will do it together the first few times."
The study will involve 260 patients with peripheral arterial disease (also known as claudication), who need to undergo a leg amputation. The nerve surgery could also benefit people who lose a leg for other reasons in the future. The first results of the new study are expected in five years.
Source: Leiden University Medical Center
06.07.2024