Predicting the future of neuroradiological imaging
As this decade ends we’ll be watching the brain think. Although anticipating very important technical developments, Professor Olav Jansen MD (right), President of the German Society for Neuroradiology (DGNR) and Director of the Institute for Neuroradiology at Schlewwig-Hostein University Hospital in Kiel, Germany, foresees even more important crucial advances in stroke therapy

Speaking of potential advances for neuroradiological imaging, Professor Olav Jansen says: ‘As far as diagnostic imaging is concerned, MRI is without a doubt in the focus.’ He also expects molecular imaging techniques that visualise morphology as well as function will become available for clinical use by the end of the decade. So far, research into physiological processes and disease diagnoses at the molecular level are limited to animal studies. ‘In the end, we need to go beyond morphology, beyond watching the brain think toward visualising brain functions,’ he stresses.
There are two routes that lead towards molecular imaging, the professor explains, one of these being increased resolution: ‘I’m convinced we will see 7-Tesla imaging, at least with regard to the central nervous system (CNS), in clinical use.’ The other route is the development of new imaging methods, such as magnetic particle imaging, in which dynamic body processes are imaged in the MR scanner without radiation exposure for patient and examiner. Last year, the German Federal Ministry for Education and Research founded MAPIT (magnetic particle imaging technology) to promote the development of MPI. Other promising examples are hybrid modalities such as PET/CT and MRT/PET, the combination of computed tomography, magnetic resonance imaging and positron emission tomography.
Professor Jansen particularly forecasts significant changes in stroke therapy. ‘In the coming decade we’ll most likely see the fusion of angiography and computed tomography, which is in fact the fusion of primary cerebral imaging and therapy in one device.’
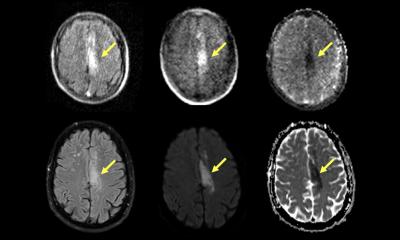
Whilst initial developments in this area are promising, image quality does not yet offer satisfactory visualisation of brain tissue; additionally, perfusion measuring is not yet available. Today, the first-line diagnostic imaging procedure for stroke patients is a CT scan. If the physician in charge decides to perform an angiography in order to open the clogged vessel, the patient is moved to a different room where the intervention is performed. In the future, CT and angiography will be done with a single system. ‘Being able to do diagnosis and therapy on the same table saves about one crucial hour; and we know: time is brain.’ Stroke –a major public health issue – is currently treated with an endovascular intervention. ‘For the past two years the trend has clearly been towards severe strokes being treated by neuroradiologists, rather than radiologists. Catheterbased therapies yield much better results than a systemic lysis,’ the professor points out. Furthermore, thrombolysis is not indicated for vessels of more than eight millimetre diameters.
According to recent studies, the outcome of angiographic neurothrombectomy in severe strokes is good in up to 60% of the cases, while thrombolysis achieves positive outcomes in 20 and 25% of cases. ‘That’s a dramatic improvement,’ he concludes. 15% of all strokes recorded in Germany are classified as severe – which means that 25,000 patients are affected each year.
‘The major public health challenge will be the setting up of structures that will provide all patients with severe stokes, all over the country, with endovascular therapy.’ Consequently the idea of local stroke units that treat all stroke patients needs to be rethought. Far better, he recommends stroke networks with one neurovascular centre that offers endovascular therapy 24/7. In this concept the problem of patient transport is less crucial, since the time window for endovascular therapy is greater than that for a thrombolysis, which needs to be initiated within four and a half hours after the stroke. Prof. Jansen: ‘For recanalisation the window is eight to nine hours – in some cases even 24 hours.’
10.07.2012