Organ donation
A business based on good faith?
Rumour had it for a while, and many found out when the bomb was finally dropped at, of all places, the Congress of the International Transplantation Society, held in Berlin this July – the waiting list for donor organs in the database of the Eurotransplant Foundation had been manipulated.
A transplant surgeon at the University Hospital Göttingen in Germany had forged dialysis and examination results to give a number of his patients – currently around 25 – improved slots on the waiting list and thus increase the number of his operations. Why? Transplant surgeons’ salaries were then volume based, which in future will not be the case. However, in the country’s largest transplant clinic at Hanover Medical School (MHH), a press officer stated that such performance-related contracts for doctors never existed at their clinic. So was this a systems error only in Göttingen; an individual single case in Europe? All hospitals have their own safeguards against manipulations, but when it comes to the assessment of patients to determine the urgency of transplantations, many doctors still advocate a ‘Four Eyes Principle’, i.e. diagnosis made by two doctors – which obviously requires more resources.
So far, there has been no proof of any financial damage or kickbacks; however, the Public Prosecutor’s Office is investigating whether charges can be brought for involuntary manslaughter and also whether other doctors were involved in manipulation. Could this, therefore, be just the tip of the iceberg? Notwithstanding, the breach of trust, particularly among the most severely ill patients, will be almost impossible to atone for – and this also goes for the millions of potential organ donors whose ethical and psychological concerns about the donation of their own body parts the Government had been trying to allay with an amendment to the law.
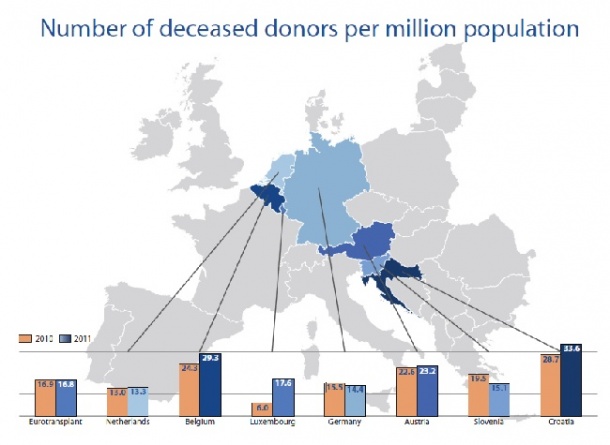
In June, the majority in the Federal German Council (Bundesrat) decided that, in future, from the age of 16 everyone with medical insurance should be regularly consulted as to whether they would donate their organs after their death. This solution is to be part of the new transplant law. Different rules apply in other European countries, and the advantages and disadvantages of various solutions and models remain controversial. However, across the board the demand for donor organs is significantly higher than the supply. In many western and central European countries, including Spain, Austria and Portugal, organs are removed from all suitable bodies unless a person had specifically objected to this before their death. These countries have an average of 21 donors per one million inhabitants. In countries with less pressure the rate is around 15 donors per million inhabitants.
To remove the finality from this presumed consent solution it has been modified in some countries, where relatives can now veto organ removal after a person’s death. This ruling applies in several European countries, including Italy and France. The Eurotransplant Foundation is responsible for the allocation of donor organs in its member states, Belgium, Germany, Croatia, Luxembourg, The Netherlands, Austria and Slovenia. It cooperates closely with the organ donor organisations, transplant centres, laboratories and hospitals. Foreigners not from one of those countries generally have no entitlement to the donor organs. However, recently this provision has also been undermined by financial remuneration of medical practitioners, in public as well as private sectors, in Frédéric Valletout’s view, should be modified and be less dependant on the volume of activity. This is slowly being introduced to general practitioners and pharmacists. In the case of hospitals, a number of options are possible: for instance a regressive fee after a certain number of interventions by one given medical team, or a lump sum allowance for small hospitals, so that they would not be tempted to inflate medical acts in order to balance their budget. doctors – in the shape of a kidney in a suitcase on its way to Saudi Arabia. The allocation of organs is based exclusively on medical and ethical criteria. Four general principles are important for allocation: The success predicted after transplantation, the urgency as determined by experts, the waiting time and the national organ exchange balance. The result to be expected after transplantation is, among others, predicted based on the donor’s and recipient’s individual characteristics after computer comparison. After the staff runs a computer comparison with the match list, the central Eurotransplant office offers donor organs to the transplant centre with the patient highest up the waiting list. To play side, the transplant centre with the patient ranked second highest on the list is also made a non-committal offer. After acceptance of the organ by the responsible doctor, the organ removal and transport is organised. There are around 16,000 patients on the central waitlist. This large number of patients makes it possible to allocate almost all donor organs to a suitable recipient – around 7,000 a year.
Thanks to international cooperation the chances for patients with the most urgent needs are increasing. Solidarity among the member countries, with their c. 125,000 million inhabitants, additionally makes it possible to help specific groups of patients such as children or patients with rare blood groups or tissue types.
The 72 transplant centres in the member states of the organisation input all important characteristics of patients waiting for an organ transplantation into the database of the central office, which is staffed 24/7. As soon as a donor has been found their characteristics are also included in the central database. Then the race against time begins. After removal, donor organs need to be transplanted within several hours, making the seamless organisation and allocation of the organ and the transport to its destination essential. This responsibility is increasingly being transferred to transplant coordinators in hospitals. The ETCO (European Transplant Coordinators Organisation) offers the necessary training for the CETC qualification (Certificate of European Transplant Coordination) at a cost of €400. Eurotransplant is ISO 9001 certified and is audited by independent organisations on an annual basis.
03.09.2012