Body dysmorphic disorder
Online therapy can help
Internet based cognitive behavioural therapy (CBT) can help people affected by body dysmorphic disorder, finds a study published by The BMJ today. This is the largest clinical trial of body dysmorphic disorder ever conducted, and the first to evaluate the effect of an internet based programme for the condition.

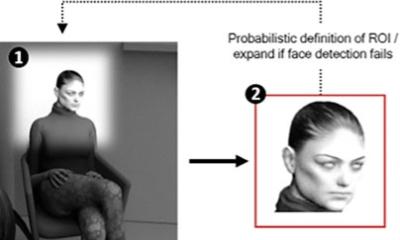
Body dysmorphic disorder (BDD) is a common anxiety disorder that causes a person to have a distorted view of how they look and to spend a lot of time worrying about their appearance. If left untreated, it can lead to hospitalisation, substance dependence and suicide.
CBT is an effective treatment, but most affected people do not have access to it. The UK government’s mental health strategy recommends the increased use of information and communication technology to improve care and access to services.
So a team of researchers based in Sweden and the UK set out to evaluate the effectiveness of a therapist guided internet based CBT programme for body dysmorphic disorder (BDD-NET) compared with online supportive therapy.
The study involved 94 adult patients with a diagnosis of body dysmorphic disorder who randomly received either BDD-NET or supportive therapy for 12 weeks.
None of the participants had any face-to-face contact with a therapist during treatment and both groups were followed for 3 months after the end of treatment.
BDD-NET resulted in significant improvements in symptom severity, depression, and quality of life compared with supportive therapy. These gains were maintained for at least three months after the end of treatment.
At that point, 56 percent of those receiving BDD-NET were classed as responders (defined as a 30 percent or more reduction in symptoms on a recognised scoring scale) compared with 13 percent receiving supportive therapy. And 39 percent of those receiving BDD-NET no longer met diagnostic criteria for body dysmorphic disorder.
Participants in the supportive therapy group who crossed over to BDD-NET after six months also improved their symptom scores.
No serious adverse events were reported, and most participants were satisfied with BDD-NET, despite no face to face contact with a therapist, and deemed the treatment as highly acceptable.
Despite some study limitations, the authors say BDD-NET “has the potential to increase access to evidence based psychiatric care for this mental disorder, in line with NICE priority recommendations.”
BDD-NET could be particularly useful in a stepped care approach, they add, “where mild to moderately affected patients can be offered BDD-NET by their general practitioner, or other health professionals, thus freeing resources for more severe and complex patients to be treated in specialised settings.”
Source: The BMJ
03.02.2016