New European guidelines on heart attack management put emphasis on speed of action
New guidelines from ECR
Timing, emergency network, reperfusion therapy are central to new recommendations for the management of heart attack which have been developed by a Task Force of the European Society of Cardiology (ESC) and were issued on the 14th November.
The guidelines state that “a well-functioning regional system of care... and fast transport to the most appropriate facility is key to the success of the treatment.”
Professor Frans Van de Werf (Leuven, Belgium), chairperson of the Task Force, describes the guidelines as “important” and says their broad uptake and adoption would make a “huge difference” to heart attack survival rates.
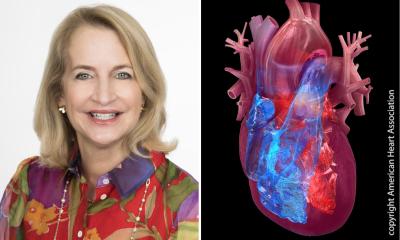
The new guidelines cover management of STEMI (ST-segment elevation acute myocardial infarction) a common type of classical heart attack. Approximately one-third of all acute coronary events are diagnosed as STEMI.
Although precise numbers are missing, it is likely that 30-50% of victims of heart attack die before reaching the hospital, most of them in the first hours after the onset of symptoms. While this mortality rate has remained fairly constant in recent years, survival rates in hospital have markedly improved – from 75% in the 1960s to around 95% today.
The introduction of coronary care units, new techniques in coronary intervention and treatments to dissolve blood clots (thrombolysis) have all improved in-hospital care.
The principal features of the new guidelines – and the major changes since the previous edition of 2003 – relate to emergency systems and a speedy emphasis on reperfusion therapy, performed either by “percutaneous coronary interventions” (PCI, with balloon angioplasty and stent) or thrombolysis treatment (with clot-dissolving drugs).
Key to management, say the guidelines, is early diagnosis and risk assessment after “first medical contact” (FMC).
• Primary PCI* is the “preferred treatment” if available within two hours of FMC.
• If PCI is not possible within two hours, pre- or in-hospital thrombolysis should be performed as soon as possible after FMC (and within 30 minutes at the latest).
*Primary PCI is defined as angioplasty and/or stenting without prior or concomitant thrombolytic therapy. It is the preferred therapeutic option when it can be performed expeditiously by an experienced team.
The shorter the delay, the better the outcome –FMC-to-balloon should be within two hours “in all cases”. However, the guidelines add that only hospitals with an established interventional cardiology programme – 24/7 - should use primary PCI.
The guidelines also recommend that most patients, following successful thrombolysis, should be routinely referred for angiography, so the condition of the coronary arteries and heart muscle can be assessed and long-term risks and treatments determined.
Professor Van de Werf concedes that not all hospitals or all regions have the emergency networks or PCI facilities recommended in the guidelines. Indeed, current registry data suggest that around 20-30% of all STEMI patients in Europe still receive no reperfusion therapy. However, adherence to the guidelines, he suggests, could “dramatically” improve STEMI patient survival.
The ambulance service is also crucial to improving survival rates – for speedy transfer, defibrillation if needed, diagnosis by ECG, early thrombolysis therapy if needed, and early alert to the hospital. The guidelines recommend that an ambulance should be available within 15 minutes of a call and all should be equipped with 12-lead ECG. Also recommended is that the techniques of basic life support should be part of the school curriculum.
Coronary heart disease is the single most common cause of death in Europe, accounting for 1.95 million deaths in Europe each year. Over one in five women (23%) and over one in five men (21%) die from the disease. Importantly, 14% of deaths before the age of 65 in men and 17% of deaths before the age of 65 in women are from CHD (European cardiovascular disease statistics, 2005)
An electronic copy of the guidelines will be available here (http://www.escardio.org/guidelines-surveys/esc-guidelines/Pages/acs-st-segment-elevation.aspx)
19.11.2008