Credit: Medical University of South Carolina
News • Neuroimaging
Stroke: MRI scan in an ambulance
Minutes matter when the brain is being deprived of oxygen. Doctors at MUSC Health's Comprehensive Stroke Center constantly work with their community hospital colleagues on initiatives to cut down the steps that need to happen between the time a stroke patient is wheeled through the ambulance bay until treatment can begin—for example, by developing a TeleEMS program so emergency medical technicians can consult with stroke specialists while inside a patient's home or the back of the ambulance.
Some things still need to happen at the hospital before treatment can begin, though, like scans of the brain to confirm a stroke and determine what type it is. But neuroradiologist Donna Roberts, M.D, wondered if a new portable MRI that she hopes to use in space might also be of use to patients in rural areas of South Carolina.
"I realized that if you have a scanner that can be used in extreme environments such as space, it can also be very useful for patients here on Earth," said Roberts, who studies how zero gravity and microgravity affect astronauts' brains.
To that end, she got together with Christine Holmstedt, D.O., medical director of the Comprehensive Stroke Center; Sami Al Kasab, M.D., associate medical director of the MUSC Health Teleneuroscience Program; and Michael Haschker, manager of telehealth technologies in the MUSC Health Center for Telehealth, to test the idea.
If it were possible to do an MRI scan in the ambulance, then not only would doctors be better prepared when the ambulance arrived, but the stroke specialists could determine whether the patient could be treated at a community hospital or would need to go directly to a specialized stroke center.
Haschker then recruited Lt. Dale Hewitt of Georgetown County Fire/EMS to help with the demonstration. Hewitt and his wife, Jessica Hewitt, R.N., a nurse leader in the Emergency Department at Tidelands Georgetown Memorial Hospital, were the catalyst for the development of the TeleEMS program, and Dale Hewitt jumped at the chance to volunteer his time driving an ambulance around Charleston while the MUSC team tested whether an MRI scan could be successfully completed in the back of a moving ambulance.
Spoiler alert: It can.

Credit: Medical University of South Carolina
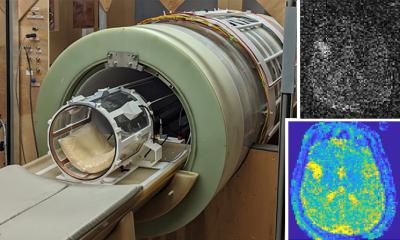
The team used a portable MRI developed by Hyperfine. "Portable" in this case is a relative term. The machine is 1,400 pounds and roughly the size of an office printer turned on its side. But that still makes it smaller than the average MRI machine. It's designed to be wheeled around a hospital to conduct brain scans at the bedside for patients who can't be moved.
"What I was completely impressed by is that it has automatic motion correction," Roberts said. "And so, as we're driving along in the ambulance, and we could see that as we bounced over the roads you could see the scanner actually move.
"So the question was, would it still be able to function and acquire diagnostic images? That was the biggest thing that this demonstration showed, is that the scanner itself was able to sense the motion and correct that in real time and so the pictures came out crystal clear. We were amazed by how nice the pictures were," she said.
Some areas have started deploying mobile stroke units, which are ambulances with CT scanners, a critical care nurse and a CT technician in addition to a paramedic. While these units have been shown to improve patients' outcomes by decreasing the time to treatment, according to a recent report in the New England Journal of Medicine, they are expensive at $600,000 to $1 million per unit, Holmstedt said.
A portable MRI machine would be a fraction of that cost, the team said, and would bring the advantages of MRI scanning.
Recommended article

Article • Act fast, save lives
Mobile stroke units: when emergency medicine hits the road
Speed in treatment of ischemic stroke can mean the difference between successful recovery versus permanent disability caused by brain tissue damage or death. Time is of the essence to perform thrombolysis with a tissue plasminogen activate (tPA), a protein that can dissolve blood clots causing the stroke or intra-arterial thrombolytic therapy (IAT) because of large-vessel occlusion.
MRI, unlike CT, doesn't use radiation, so there would be no radiation exposure to the patient or the first responders, Al Kasab said. An MRI is also a more accurate diagnostic tool for stroke, he said. It can show smaller blockages, and, in the case of strokes caused by blood clots, it would allow doctors to determine whether a patient needed the clot-busting drug tPA, which can be administered at community hospitals, or a thrombectomy, a surgical procedure to remove the clot.
Al Kasab said that the current triage system calls for patients to first go to a tPA-capable center and receive tPA. But although tPA works well for small blood clots, it's much less likely to work on large clots.
"So, if you can imagine, if a patient has a large clot in the brain, they go to the tPA center and get tPA and then transfer here. By the time they get here, there is a very good chance that those patients will no longer be eligible for thrombectomy because there's already so much damage," he said.
Reducing the time before treatment begins isn't simply a matter of reducing the number of stroke deaths in South Carolina. It's also about reducing the severity of disabilities for those who survive. "We know for every 15-minute reduction in 'door-to-needle time' there's significant improvement in patient outcomes, including reduction in disabilities and reduction in mortality," Holmstedt said.
Haschker said that reducing the time to treatment is especially important for those who live in rural areas. "South Carolina is a leader in stroke, but we're also a leader in stroke care. We want to have one of the most advanced stroke care programs in the United States, and we have a lot of data, so we know that a lot of care can be delivered when the patient is in the ambulance," he said.
The MUSC team will be writing up a report of their practical demonstration. They think it's the first MRI scan performed in an ambulance. "We think we're the first—but we know we're the first to ever do an MRI scan on the Cooper River Bridge," Haschker joked.
The team is also grateful to staff members of the facilities and supply teams who helped to load the machine into the ambulance. Haschker envisions that if this idea were to become a reality, there would be ambulances equipped with MRI scanners strategically situated so that they could respond to potential stroke calls.
In fact, Holmstedt hopes to run a pilot program in Charleston County to determine the feasibility and potential lifetime cost savings per patient.
Source: Medical University of South Carolina
05.01.2022