Article • Regulatory issues for AI and digital pathology
IVDR: a complex issue and a 'missed opportunity'
The regulatory landscape covering digital pathology and AI is proving complex, challenging and more extensive than many of those involved in the field initially believed. Despite a five-year transition period for In-vitro Diagnostic Medical Device Regulation (IVDR), one leading expert fears many actors in the field are still not prepared for the regulations coming into force, even with a possible one-year deadline extension.
Report: Mark Nicholls
Image source: Medical University Graz
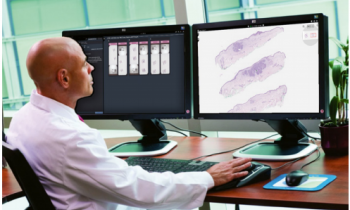
The regulatory challenges were explored at the 8th Digital Pathology & AI Congress in London by Professor Kurt Zatloukal, Head of the Diagnostic and Research Centre for Molecular Biomedicine at the Medical University Graz, Austria. During the session, he examined how the IVDR performance requirements might shape digital pathology and AI-supported diagnostics.
Being in place since 2017, the transition period for the regulation is scheduled to end in May 2022. This, however, seems increasingly unlikely, and the expert predicts that the deadline will have to be extended – with the markedly increased prerequisites of the IVDR being the main reason: ‘It is a much broader and more demanding regulation than the previous directive, requiring that 80% of all diagnostics that are on the market today in Europe need additional data in order to comply,’ he said. ‘This includes increased documentation on scientific evidence, analytical and clinical performance.’ Further challenges are expected to stem from the introduction of a new risk classification system and the inclusion of software – including AI-based analysis technology – in the scope of the IVDR.
‘Black box’ AI solutions not accepted
Prof Zatloukal sees potential for complication in the need to show scientific validity associated with a clinical or physiological state. While this is easy to establish for lab medicine, it might not be so clear when talking about digital pathology and AI, he points out. ‘What it means, for example, is that it is not acceptable that an algorithm acts like a “black box”. It must be made clear what features are recognised and how these features are associated with a clinical or physiological state to demonstrate compliance with this regulation.’
Recommended article

News • WHO global report
The six guiding principles for AI in healthcare
Artificial Intelligence (AI) holds great promise for improving the delivery of healthcare and medicine worldwide, but only if ethics and human rights are put at the heart of its design, deployment, and use, according to new WHO guidance.
‘Another aspect is the general performance requirement and the need to show that a device is suitable for a certain purpose,’ the expert continued. For digital pathology and diagnostic AI algorithms, this means that analytical and clinical performance for the device has to be demonstrated. ‘That also includes the quality of the original specimen that is analysed, because for an algorithm used to analyse digital images, it has to demonstrate that the algorithm is valid for a certain sample quality.’
Under the new regulation, AI-based algorithms for diagnostic decision-making will have a particularly hard time to attain approval, Prof Zatloukal predicts. From tissue collection, staining, and scanning, down to the question of how the results should be displayed to the pathologist – the whole workflow must be factored in. ‘Just focusing on one part without considering the other variables of a diagnostic workflow will not meet the scope of IVDR for a decision-support solution,’ he emphasised, pointing out that the landscape of in-vitro diagnostics standards is highly complex as it is.
Poor use of the five-year transition period
One standard that is highly relevant for digital pathology and AI is ISO 20166-4, which addresses the complete pre-analytical workflow for all in-situ detection techniques for diagnostics. This is especially relevant because it gives specific reference to the development of new technologies, including digital pathology and computer-based analysis of slides with classical H&E staining, immunohistochemistry, or in-situ hybridisation, the expert explained.
While one of the main objectives of the new IVDR is enhancing patient safety, healthcare systems seem to lack awareness for how much time and resources are needed to implement the necessary changes, said Prof Zatloukai. In conclusion, he believes the five-year transition period of IVDR to be a ‘missed opportunity’ for many organisations to get prepared.
Profile:
Kurt Zatloukal is Professor of Pathology and head of the Diagnostics and Research Centre for Molecular Biomedicine at the Medical University Graz in Austria. His research focuses on the molecular pathology of metabolic liver diseases and cancer as well as molecular diagnostics and machine learning approaches for digital pathology. He is a member of the Austrian Standards Institute, as well as CEN and ISO technical committees being involved in the development of a series of standards related to molecular diagnostics and in-situ detection techniques with special emphasis on the needs of digital pathology.
03.02.2022