Interventional and combined approaches show promise in advanced liver Cancer
Emerging interventional techniques appear promising for the treatment of hepatic tumours, even those at advanced stages. Attendees at the special focus session on transarterial procedures, taking place today at ECR, will find out just how far these techniques, as well as combined approaches, have gone.
Surgery and liver transplantation are being widely used to treat hepatocellular carcinoma (HCC), incidence of which has increased steadily, particularly due to the spread of the hepatitis C virus.
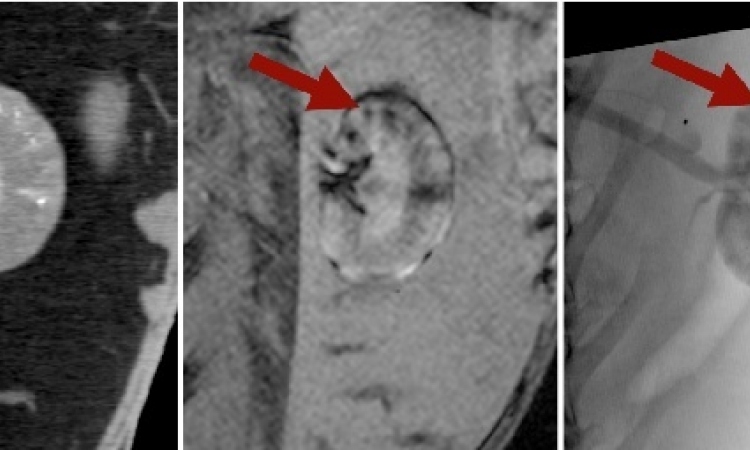
For around 80% of liver cancer patients, surgical options are no longer viable once the disease has been diagnosed, which means the patients become candidates for interventional approaches. Radiofrequency (RF) ablation is an effective option for patients with early-stage HCC, particularly if the tumour is no larger than 3–5 cm in diameter. For patients at an intermediate or advanced stage, because HCC is highly chemoresistant, the traditional method of classical systemic infusion chemotherapy is not very effective.
Chemotherapeutic agents such as doxorubicin must thus be infused locally in high concentrations into the artery supplying the tumour. After local application using a catheter, arterial flow to the tumour must be blocked by embolisation. This method, transarterial chemo-embolisation (TACE), has shown promise in randomised trials. Furthermore, drug-eluting beads allow small particles to be loaded with the chemotherapeutic agent to transport doxorubicin directly into the tumour, blocking arterial flow at the same time. Results published from a European multicentre randomised study (Johannes Lammer et al, Cardiovasc. Intervent. Radiol. 2009) show improved outcome compared to conventional TACE. Drug-eluting beads used with doxorubicin are now attracting attention as a palliative life-prolonging treatment. Compared with conventional TACE, drug-eluting beads have significantly fewer adverse side effects because the therapeutic agent remains in the tumour and does not circulate in the patient’s body.
“In terms of therapy options, this is likely to be news to many radiologists. It’s important for them to know that even for patients with advanced tumours there is now a viable treatment,” said session moderator Prof. Johannes Lammer, director of cardiovascular and interventional radiology at Vienna’s Medical University.
Another study published last year in Cardiovascular Interventional Radiology by Dr. Katarina Malagari demonstrated that chemo-embolisation using drug-eluting beads was significantly better in terms of subjective patient response and time to progression compared to bland embolisation.
Also under evaluation in large European multicentre studies is another therapeutic option that involves radioembolisation using beta-emitting Yttrium particles injected into the tumour-feeding artery. This highly effective local radiation can kill the tumour cells without damaging the liver. Additionally, therapies combining TACE with drug-eluting beads and RF ablation are being studied in a multicentre randomised trial now in its second year.
“TACE can first reduce the size of the tumour, so that those patients who aren’t candidates for surgery, or whose tumours are a little too large for ablation, can still profit from curative ablation rather than palliative treatment,” Lammer said.
“The efficacy of a combination therapy, including RFA plus the intra-arterial administration of drug-eluting beads has been recently demonstrated, while the use of intravenously administered, thermally sensitive drug carriers is currently being explored,” added Professor Riccardo Lencioni, Director of Diagnostic Imaging and Intervention at Cisanello University Hospital in Pisa. Experimental studies in animal tumour models have shown that lowering the temperature threshold at which cell death occurs by combining sublethal heating with cell exposure to chemotherapeutic agents is an attractive alternate strategy for increasing tumour necrosis.
Despite the advances in local treatment, the long-term outcome of treated patients remains unsatisfactory because new tumours emerge within five years in about 80% of the cases. Adjuvant molecular targeted therapies with anti-angiogenic and anti-proliferative activity may prove useful in preventing early recurrence after successful ablation. Clinical trials of these methods are currently ongoing. Surgery remains the gold standard in HCC therapy. But if research over the next couple of years proves that a combined approach is effective, its routine use in the clinical setting will increase, to the benefit of patients, experts predict.
07.03.2011