Infant receives first systemic therapy to treat RDEB
Children with recessive dystrophic epidermolysis bulosa (RDEB) lack a protein that binds the skin to the body, resulting in fragile skin that sloughs off with little movement or friction.
In the most severe cases, the skin also sloughs off inside the body, affecting the mouth, oesophagus and gastro-intestinal tract. EB is genetic and severe forms are fatal. Those who live to be young adults develop squamous cell carcinoma.
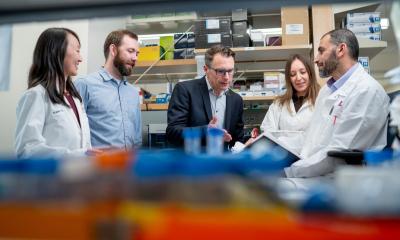
Now the first bone marrow and cord blood transplant to treat RDEB has been carried out by physicians at the University of Minnesota Children’s Hospital, Fairview, with the collaboration of researchers at Columbia University, University of Minnesota, on an 18-month-old boy suffering the most severe form of RDEB.
With the help of an EB mouse model the researchers corrected the disease in mice using bone marrow. They tested various types of adult stem cells to determine which would promote the development of type VII collagen — a protein that patients with RDEB lack. One type of immature cells from bone marrow proved the best at producing binding fibrils that hold skin and body together.
This is the first approach to EB from a systemic perspective, using transplant as a method to rid the body of the defective blood system and replace it with a healthy
blood system that produces type VII collagen.
The child received both umbilical cord blood and bone marrow from a perfectly matched sibling. If the results mimic the animal model, doctors anticipate the healthy blood system will aid in the skin’s ability to produce type VII collagen necessary to anchor the skin and lining cells of the gastrointestinal tract to the body. Doctors anticipate in early 2008 — approximately 100 days after transplant – they will be able to judge whether this treatment helped.
The paediatric BMT programme at the University of Minnesota Children’s Hospital, Fairview, is internationally recognised for pioneering umbilical cord blood and bone marrow transplantation, including the world’s first successful BMT in 1968. In 2000, a team led by John E Wagner MD, professor of Paediatrics and director of the Division of Haematology, Oncology, and Blood and Marrow Transplantation and director of clinical research of the Stem Cell Institute, University of Minnesota, performed the first umbilical cord blood transplant from a sibling donor ‘created’ after embryo selection. The programme leads the nation in the use of umbilical cord blood in the treatment of adults and children and in the development of innovative treatments of various rare genetic diseases such as adrenoleukodystrophy (ALD) and Fanconi anaemia.
Of this recent transplant, Professor Wagner said: ‘Our goal is to determine the usefulness of stem cells, whether from the umbilical cord blood or adult tissues like bone marrow, in the treatment of human disease. Hundreds of thousands of children and adults are waiting for new breakthroughs in stem cell research, and time is never enough. In two years, the team was able to move this project forward remarkably fast — from testing in animal models to treating patients. Time will tell whether this risky treatment will work as effectively in humans. But, RDEB is a horribly debilitating, life-threatening disease with no existing curative therapy.’
Maria Hordinsky MD, head of the Department of Dermatology at the University of Minnesota and a member of the care team, added: ‘This represents a real change in thinking within the dermatological community. The possibility of this approach compels us to explore more broadly the way some skin diseases are typically treated.’
Source: Molly Portz, University of Minnesota
14.11.2007