Hypofractionation
Making prostate cancer therapy more effective, more comfortable for patients and less expensive for society? Dose escalation, up to 80 Gy and above, may be necessary to successfully treat localised prostate cancer with radiotherapy (RT).

‘This is a challenge for radiation oncologists in their rearch for an optimal treatment of a movable, centrally-located, almost spherical target surrounded by dose-limiting critical organs such as the rectum, bladder and femoral necks’, says Professor Raymond Miralbell head physician of the oncology radiation department at Geneva’s university hospital.
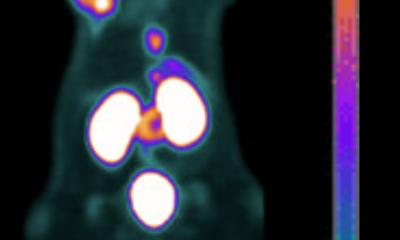
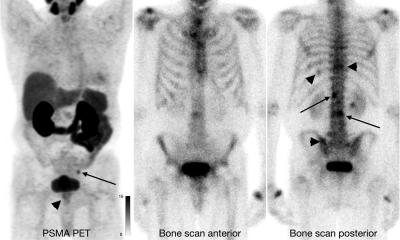
The future for curative radiotherapy for prostate cancer may be a mix of more and less: more total dose and more dose per fraction delivered in less number of fractions (hypofractionation), to a lesser treatment volume boost to the dominant tumour-bearing region inside the prostate. In the last two decades hypofractionated high-dose rate brachytherapy has been successfully employed in delivering a focused boost after standard fractionated external beam RT to the prostate pelvic nodes. External stereotactic body RT (SBRT) can be used as a contemporary dose escalation approach comparable to HDR-BT, to escalate the dose to the prostate non-invasively and in optimal radiation safety conditions.
Prof. Miralbell’s benefits in the use of this therapy include: Moderate hypofractionation (from 2.5-3.5 Gy) has been a standard treatment procedure in the UK, Canada and Australia for many years. Treatment delivery is fast, with reduced numbers of fractions being better for patients and perhaps less expensive Advances in image-guided target conformation prevent normal tissue surroundings from large radiation doses and minimise potential toxicity Hypofraction is radiobiologically sound against prostate cancer cells with relatively low radiosensitivity and high repair capacity of sub-lethal damage. Indeed if, for instance, after delivering a standard dose per fraction of 2 Gy the survival fraction of the tumour cells would be about 75% after twice the dose per fraction, i.e., 4 Gy, the survival fraction might be only 15%, a killing effect of five times more cells by just doubling the dose. ‘Hypofractionation is the challenge to deliver very high doses to very small volumes, very well defined and very well guided by the imaging. So we take the benefits of radiobiology and technology’, the professor explains.
Just a few preliminary studies have recently shown the potential of hypofractionation in improving the therapeutic outcome. However, back in 2001 extreme hypofractionation began with the Novalis machine. Two weekly fractions of a very high radiation dose (i.e. 5-8 Gy) were given at the end of a standard fractionated irradiation programme of 32 times 2 Gy in daily sessions, to test the same hypofractionation concept that highdose rate brachytherapy could already obtain.
The results were very encouraging, especially considering the patients’ advanced local disease status, with an eight-year biochemical disease-free survival (bDFS) and disease-specific survival (DSS) results of 95% and 100%, respectively. Among the cured patients testosterone levels at last follow-up were back to normal in 90% of patients. 28 days in four weeks. From the literature we know that the treatment should not be excessively protracted, to avoid tumour cell proliferation during the treatment interval, which might increase the load of tumour cells to be killed by radiation,’ he explains. ’ Most average risk tumour cell proliferation begins around days 30 to 35 after the first day of radiotherapy; therefore it is important not to extend treatment beyond four weeks. Although, patients treated according to the first group (nine days) may show a worse tolerance due to the short treatment time, patients treated along the more protracted second arm (28 days) may risk a lower control probability because of an accelerated repopulation of tumour cells. ‘We want to be sure that the effect will be as good as we expect, thus a rate of 90-95% cure.’
Extreme hypofractionated stereotacticguided IMR to the dominant tumour-bearing region within the prostate is feasible and shows an acceptable toxicity as well as an excellent outcome. Accurate target definition with functional MRI, an efficient immobilisation device, and reliable control of internal organ motion, are all key factors to assure the highest precision in this treatment technique. Additionally, optimal dose homogeneity within the target, an OTT of five weeks or less, and fraction treatment duration of 15 minutes or less, should be attempted to gain the maximum benefit of SBRT for prostate cancer.
31.05.2012