News • Study asks neurosurgeons
How old is too old to perform brain surgery?
People sometimes joke that easy tasks are “not brain surgery.” But what happens when it actually is brain surgery? How old is too old to be a neurosurgeon?

In a new Mayo Clinic Proceedings study, most neurosurgeons disagreed with an absolute age cutoff, but half favored additional testing for neurosurgeons 65 and older. Some professions, including commercial pilots, FBI agents and air traffic controllers, have mandatory retirement ages. This study is the first to survey neurosurgeons on their attitudes toward ceasing practice and testing in late career. “With an aging physician workforce nationwide, this study’s intriguing responses deserve reflection by the neurosurgical community,” says senior author Fredric Meyer, M.D., executive dean of education, Mayo Clinic, who is executive director of the American Board of Neurological Surgery. Dr. Meyer is the Juanita Kious Waugh Executive Dean of Education and the Alfred Uihlein Family Professor of Neurologic Surgery.
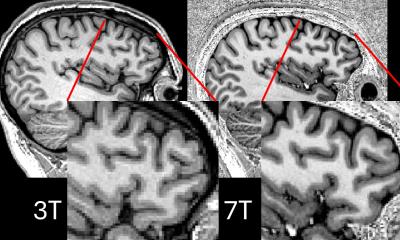
Surgical simulator training and testing may become essential in continuing assessment of a surgeon’s technical and cognitive competency
Fredric Meyer
“It’s important to focus on patient safety and also assess a neurosurgeon’s capacity over time,” Dr. Meyer says. “In the future, “It’s important to focus on patient safety and also assess a neurosurgeon’s capacity over time,” Dr. Meyer says. “In the future, surgical simulator training and testing may become essential in continuing assessment of a surgeon’s technical and cognitive competency.” Training to become a neurosurgeon is a lengthy process — typically four years of medical school, seven years in neurosurgical residency and frequently an additional year of post-residency fellowship. Neurosurgeons may perform surgery on the brain, spine or any part of the central nervous system. Of 4,899 neurosurgeons surveyed, 1,449 (30 percent) responded to an anonymous and confidential questionnaire..” Training to become a neurosurgeon is a lengthy process — typically four years of medical school, seven years in neurosurgical residency and frequently an additional year of post-residency fellowship. Neurosurgeons may perform surgery on the brain, spine or any part of the central nervous system. Of 4,899 neurosurgeons surveyed, 1,449 (30 percent) responded to an anonymous and confidential questionnaire.
Most respondents, 938 (65 percent), were 50 and older. Asked how to fairly evaluate aging neurosurgeons, respondents said:
- There should be no absolute age cutoff, 956 (66 percent).
- Neurosurgeons 65 and older should undergo additional testing, including cognitive assessment or a review of cases, in addition to a standard Maintenance of Certification exam, 718 (50 percent).
- A Maintenance of Certification exam should include individual case log and patient outcome review, 766 (59 percent).
- A Maintenance of Certification exam should be tailored to accommodate the aging neurosurgeon, 606 (42 percent).
Because more than one-third of U.S. surgeons are older than 55, the issues raised in the study will be important to other surgical disciplines, notes Kerry Olsen, M.D., a Mayo Clinic otorhinolaryngologist, in an accompanying editorial. “Deciding when to end one’s surgical practice can be an extremely difficult decision,” says Dr. Olsen, who no longer performs surgery. He suggests interventions such as assisting surgeons with ergonomics to prevent work-related injuries, asking younger colleagues for honest assessment of one’s skills, and creating opportunities for hospitals and clinics to use surgeons’ talents beyond being “captain of the operating room suite.”
Source: Mayo Clinic
16.11.2017