Image source: Shutterstock/Magic mine
News • Surprising discovery
Fatty liver disease can also affect lean people
Nonalcoholic fatty liver disease (NAFLD) is mostly diagnosed in overweight and obese people. However, severe forms of NAFLD can also be detected in rare genetic diseases such as lipodystrophy or in patients with HIV, putting them at a high risk for developing liver failure, diabetes and cardiovascular diseases.
Norbert Stefan and colleagues have now detected a yet unknown cause of NAFLD in lean people. They report a case of a woman who received immune checkpoint blockade therapy for skin cancer, which may have triggered inflammation of her subcutaneous fat, resulting in a dramatic loss of fat mass and severe NAFLD.
The researchers published their findings in the journal Annals of Internal Medicine.
The world-wide epidemic of NAFLD is thought to mainly be driven by an unhealthy lifestyle with little physical activity and a diet high in saturated fats, sugar and fructose. In these overweight and obese patients, weight-loss brought about by lifestyle modification is considered most effective and safe to treat NAFLD and reduce the risk of advanced forms of liver diseases, such as cirrhosis or liver cancer, type 2 diabetes and cardiovascular diseases (CVD). However, NAFLD can also be found in lean people. These patients either have genetically-determined lipodystrophy, acquired lipodystrophy syndromes or HIV-lipodystrophy, which are all characterized by a dramatic reduction in fat mass under the skin and an increase of fat inside the abdomen and in the liver.
Thomas Eigentler and Diana Lomberg from the Department of Dermatology of the University Hospital of Tübingen, Germany, and Jürgen Machann and Norbert Stefan, from the Department of Internal Medicine IV of the University Hospital of Tübingen, the Helmholtz Zentrum München and the German Center for Diabetes Research (DZD), have now detected a novel cause of acquired lipodystrophy. They report the case of a 45-year-old woman having malignant melanoma, a skin cancer, which was effectively treated with the programmed cell death protein 1 (PD-1) inhibitor Nivolumab. This and other so-called “checkpoint inhibitors” have revolutionized the treatment of cancer, especially malignant melanoma.
It is important that clinicians treating patients with checkpoint inhibitors should be aware of a newly-identified adverse event associated with such therapy
Norbert Stefan
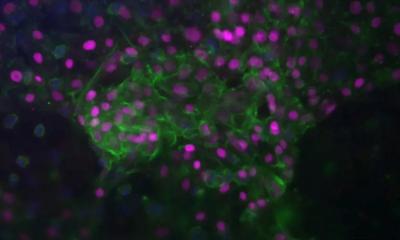
However, therapy with these checkpoint inhibitors is also associated with adverse events that commonly affect the skin, gastrointestinal tract, lungs and endocrine system. Towards the end of treatment with Nivolumab, Stefan and colleagues found in their patient very high levels of lipids, a newly developed diabetes and a severe form of NAFLD. This was completely unexpected, particularly because their patient lost 31 kg of body weight. Tissue biopsy of her subcutaneous fat and magnetic resonance imaging resulted in the diagnosis of acquired lipodystrophy with a severe form of inflammation of her fat. This may have been triggered by the immonomodulatory function of checkpoint inhibitors in the patient, who was previously diagnosed with asymptomatic mastocytosis, an immune-cell related disorder. Intensive pharmacological treatment, particularly with pioglitazone, which induces an increase in fat mass under the skin, resulted in that her liver fat, liver enzymes and lipid levels returned to almost normal values.
Stefan, who is a Professor of Diabetology at the University of Tübingen, and a Visiting Professor at the Harvard Medical School, Boston, concludes that “it is important that clinicians treating patients with checkpoint inhibitors should be aware of a newly-identified adverse event associated with such therapy. Inflammation of adipose tissue, resulting in severe fatty liver may occur. In such conditions specific pharmacotherapy, possibly involving mechanisms to increase the amount of subcutaneous fat mass, and, thereby, keeping the lipids in a safe storage space, may be very helpful in these patients.”
Source: University Hospital of Tübingen
04.03.2020