Image source: Gerd Altmann from Pixabay
News • AI uncovers neurological changes
Facial analysis algorithm to track Parkinson’s Disease
Parkinson’s disease (PD) is a well-studied neurodegenerative disorder that affects between 7 and 10 million people worldwide. Despite PD being a recurrent topic in the medical literature for over 200 years, its mechanisms are largely unclear, and existing treatments are aimed at improving the patient’s symptoms.
Among PD’s most common symptoms are motor problems, including as tremors, slowness, and muscular rigidity. These, combined with many non-motor symptoms, cause many PD patients to develop facial abnormalities, such as face skin problems and difficulties making facial expressions. Such problems are not to be taken lightly, as one’s face plays a crucial role not only in self-esteem, but also when interacting with others. Unfortunately, facial changes in PD patients are difficult to track and quantify with conventional techniques.
But what if artificial intelligence (AI) could provide the tools needed? In a recent study published in Brain Supplement, a team of scientists from Okayama University, Japan, tested whether modern facial detection and analysis algorithms could be useful in the context of PD. Led by Dr. Koh Tadokoro of the Department of Neurology, the team recruited 193 people, half of which were PD patients at different stages of the disease and the other half were healthy control subjects. The subjects were taken to a consulting room in the University’s clinic, and the researchers took a single photograph of their face without giving any special instructions.
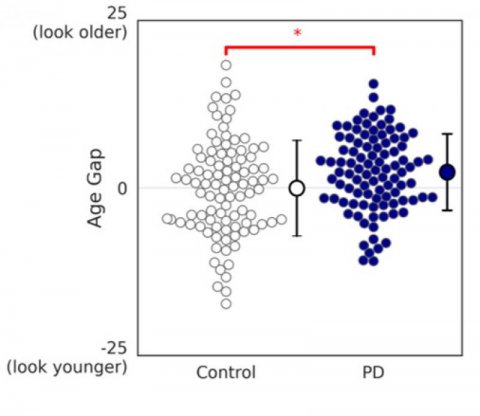
Credit: 2021 Brain Supplement
Once the pictures were taken, the team used commercially available AI software to detect the subjects’ faces and analyze some of their attributes; namely apparent age, expressed emotion, and facial skin condition. Through statistical analyses, they explored whether AI-based algorithms could find significant differences in these attributes between the control group and the PD group.
Interestingly, the age gap, which is the apparent age estimated by the software minus the real age of the subject, was a factor that differed between both groups. On average, the age gap for PD patients was higher than for healthy subjects, revealing that the former tended to look slightly older than their actual age in the eyes of the AI. In addition, the facial expression of PD patients was more likely to be classified as “expressionless” compared with healthy subjects, who were significantly more likely to carry an expression classified as “happiness.” On the other hand, in terms of skin condition, the researchers found no noticeable differences between both groups.
Overall, the strategy adopted in the study and the results gathered could pave the way for incorporating AI-based software into future research on the symptoms of PD. The approach the team used is relatively simple and cost-effective, as Dr. Tadokoro explains: “Whereas most previous studies evaluated the facial changes caused by PD during movement or tasks, we found evidence of specific facial changes based solely on a single photograph using modern AI.” Additionally, the team also noted some limitations of facial analysis software, such as performing worse in some regards for people with darker skin or being less accurate when estimating the age of Asians. Such problems can and should be addressed before the software is put to use in clinical research.
In short, it is possible that AI-based tools bear untapped potential for the rapid, quantitative analysis of patients with PD. Excited about the results, Dr. Tadokoro remarks: “We hope our study accelerates the use of AI technology for the diagnosis and treatment of patients with Parkinson’s and other neurodegenerative diseases.” Future researchers might want to take note of the power of AI in the context of neurological disorders to push the field forward towards a deeper understanding.
Source: Okayama University
17.03.2021