Article • Advancements in endoscopy
Enhancing diagnosis and disease monitoring for ulcerative colitis
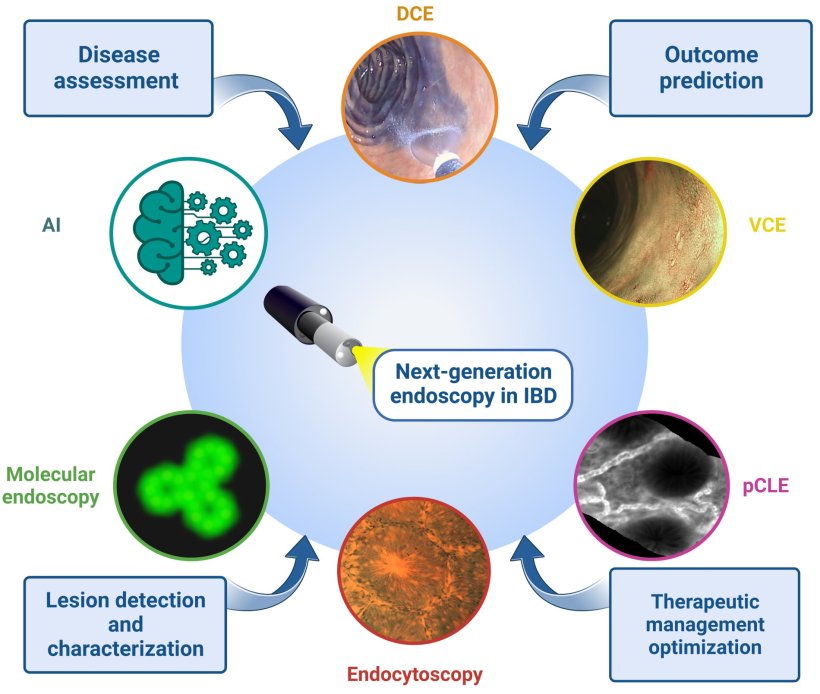
Endoscopy is pivotal in diagnosing and managing ulcerative colitis. Recent technology advances allow for early cancer detection, precise disease assessment and targeted biopsies, improving diagnosis and monitoring. The following article takes a look at the latest advancements.
Report: Bernard Banga
Ulcerative colitis (UC) is a chronic inflammatory bowel disease characterized by recurrent inflammation of the colon and the rectum. According to the recent reference book "Ulcerative Colitis", the total number of new cases diagnosed each year is approximately 38,000. In 2023, its prevalence was estimated to be 5 million diagnosed cases worldwide and increasing yearly. The chronic inflammatory stimulus in UC patients is associated with a higher risk of developing colorectal cancer as compared to the general population.
Expanding disease evaluation beyond conventional methods

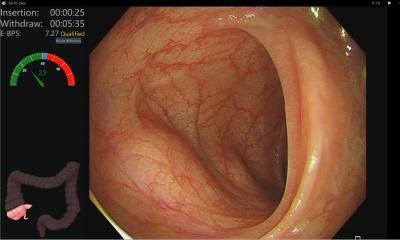
Endoscopy plays a crucial role throughout the entire course of the disease, starting from the diagnosis. ‘It is indispensable for obtaining histological confirmation, determining the extent and severity of the disease, monitoring activity, performing dysplasia surveillance and providing endoscopic treatment when possible,’ said Dr Ferdinando D’Amico, gastroenterologist at the Unit of Gastroenterology and Digestive Endoscopy at San Raffaele Hospital in Milan, Italy.
However, it faces issues like variability in scoring systems, incomplete colon assessments, limited endoscopy access in some regions, lack of standardization, and the necessity for invasive tissue biopsies for a definitive diagnosis.
In recent years, new technologies have emerged, which could potentially overcome limitations associated with conventional techniques. ‘These advancements offer the opportunity for ultrastructural, macroscopical, and even microscopical evaluation of the disease that were previously unavailable,’ wrote D’Amico in a recent article published in Biomedicines.
[Endocytoscopy enables] magnification of up to ×1440 without contrast or video processors but does not require administration of intravenous contrast or additional video processors
Ferdinando D'Amico
Two different systems can be distinguished: probe-based CLE consists of a bundle of fibre optics with a lens at its distal end, which is connected to a laser scanning unit. On the other hand, endoscope-based CLE (eCLE) involves the integration of a confocal microscope into the distal tip of a conventional endoscope. CLE and eCLE can be used to predict sustained clinical remission and a reduced need for hospitalization, steroid therapy, and surgery.
For its part, EC employs a high-powered fixed-focus lens, which can be integrated into the endoscope or utilized through a separate probe, ‘enabling magnification of up to ×1440 without contrast or video processors but does not require administration of intravenous contrast or additional video processors,’ stated D’Amico. Recently, Japanese researchers highlighted EC's accuracy in endoscopic resections, while a German team showcased its superiority over white-light endoscopy in Gastrointestinal Endoscopy.
New technologies for assessing disease activity in ulcerative colitis patients
Confocal laser endomicroscopy (CLE) and endocytoscopy (EC) provide both diagnostic information at the cellular level, allowing for the detection of microscopic changes in the mucosa that may not be visible with traditional endoscopy. Confocal laser endomicroscopy is an advanced endoscopic technique developed to capture highly detailed and magnified images of the mucosa in the gastrointestinal tract. It uses stains during endoscopy to highlight differences in mucosa and increase the detection rates for various pathologic processes. ‘This technology relies on the illumination of tissue using a low-power laser, followed by the detection of fluorescent light reflected from the tissue through a pinhole after the application of systemic or topical fluorescence agents,’ stated D’Amico.
Precision surveillance: Chromoendoscopy and autofluorescence in colitis cancer
Patients with long-standing ulcerative colitis, excluding those with limited proctitis, have an increased risk of colorectal cancer as a result of inflammation-induced carcinogenesis. ‘Recently, the availability of novel medical therapies and the implementation of improved colonoscopic surveillance have led to a reduction in colitis-associated colorectal cancer,’ explained D’Amico. As non-invasive biomarkers for colitis-associated colorectal cancer are lacking, colonoscopy remains the mainstay of colitis-associated colorectal cancer risk attenuation.
Initially, the recommended screening method was white light endoscopy (WLE) with random four-quadrant biopsies taken every 10 cm. The new technology of chromoendoscopy is providing real-time imaging of the gastrointestinal tract, allowing for the detection of abnormalities and the assessment of disease activity. Chromoendoscopy, virtual or dye, is an endoscopic technique that involves the application of topical stains or dyes during an endoscopic procedure to increase the sensitivity of the procedure by facilitating the identification of mucosal abnormalities, particularly flat or depressed lesions. Its main components include staining agents, spray catheters, virtual chromoendoscopy, mucolytic agents, and targeted biopsies.
The secondary technology of autofluorescence imaging (AFI) utilizes the properties of light-tissue interactions to enhance neoplastic tissue. Indeed, when exposed to ultraviolet or short-wavelength visible light, endogenous fluorophores (collagen, nicotinamide, flavin, porphyrins) emit fluorescence. ‘However, current data about AFI are still not available to evaluate its role in clinical practice,’ stated D’Amico.
AI-enhanced imaging shows great promise in ulcerative colitis monitoring
Artificial intelligence (AI) models are paving the way for predicting ulcerative colitis progression and pre-empting short- to medium-term disease exacerbations. Indeed, emerging as a valuable tool in inflammatory bowel disease (IBD) diagnosis and management, AI offers the possibility of the simultaneous analysis of miscellaneous biological data ‘by permitting a large-volume input for machine-learning models, such as cross-sectional imaging, endoscopic and histological imaging, inflammation biomarkers, as well as gut microbiota composition and gene expression,’ said Dr Monica State, from the gastroenterology department at Colentina Clinical Hospital, Bucharest, Romania. AI tools can therefore potentially increase the efficiency and accuracy of endoscopic diagnosis and treatment of ulcerative colitis.
The future of medical diagnostics may soon incorporate AI-based prognostic models that blend endoscopic, clinical, histological, laboratory, and imaging data, alongside transcriptional, proteomic, and microbiome biomarkers
Ferdinando D'Amico
The gastroenterology and endoscopy team at San Raffaele Hospital reported that AI-driven applications in digestive endoscopy for ulcerative colitis offer significant advantages. These technologies can accurately differentiate between remission and non-remission using static images, conduct real-time endoscopy, even in the presence of patient movement, various bowel conditions, peristalsis, and biopsy-related mucosal damage. Additionally, they enhance histological predictions, marking a notable stride in medical technology.
‘The future of medical diagnostics may soon incorporate AI-based prognostic models that blend endoscopic, clinical, histological, laboratory, and imaging data, alongside transcriptional, proteomic, and microbiome biomarkers,’ said D’Amico. However, despite their potential to process extensive datasets, these emerging techniques are yet to become mainstream in clinical practice due to a lack of standardization. It's important to note that these advanced models provide predictions rather than definitive conclusions, introducing ethical considerations into their application.
Efforts are underway to address this issue. Organizations like the Consolidated Standards of Reporting Trials–Artificial Intelligence (CONSORT-AI), Standard Protocol Items: Recommendations for Interventional Trials–Artificial Intelligence (SPIRIT-AI), and the European Society of Gastrointestinal Endoscopy (ESGE) are taking initial steps towards establishing guidelines for AI model development and clinical utility. The medical community eagerly anticipates prospective, multidisciplinary, and multicentre studies to assess the potential.
Profile:
Dr Ferdinando D'Amico is a gastroenterologist at the Gastroenterology and Digestive Endoscopy Unit, led by Prof. Silvio Danese at IRCCS San Raffaele Hospital in Milan, Italy. Since 2020, D'Amico has been specializing in digestive diseases at Humanitas University in Milan. His clinical interests encompass chronic inflammatory bowel diseases like Crohn's disease and ulcerative colitis, along with Diverticular disease, irritable bowel syndrome, gastroesophageal reflux disease, dyspepsia, and endoscopy. With 85 scientific articles and book chapters to his name, D'Amico is a prominent figure in the field, frequently speaking at international conferences.
13.05.2024