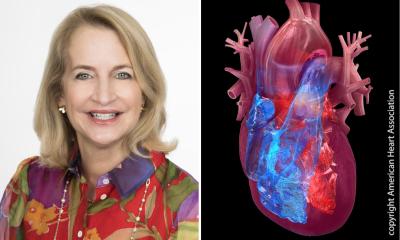
CVD and women
by Silvia Priori
New initiative aims at clarification and education.

Cardiovascular disease (CVD), which includes coronary heart disease and stroke, kills more people of both sexes than all cancers combined. However, according to public awareness surveys, women think cancer - particularly of the breast - is a greater risk for them. The truth is that CVD kills a higher percentage of women (55%) than men (43%) in Europe and accounts for more deaths than all cancers combined. It is also notable that although men suffer strokes, women are more likely to die as a result of a stroke.
To address this, at a recent meeting of its 49 national cardiac societies the European Society of Cardiology (ESC) launched the Women at Heart initiative, aimed at medical professionals, because, the ESC points out, women are under-represented in clinical trials and their CVD clinical manifestations are less well charted and outlined to the medical professional in their initial or ongoing training.
Apart from increasing awareness across Europe, among many other activities will be an analysis of ESC Euro Heart Survey databases to obtain specific data on women and CVD, such as the differences between women and men in specific disease and treatment areas. Results from these analyses will be presented at the Euro Heart Survey Symposium at the ESC Congress in September.
Professor Silvia Priori, of the Fondazione Salvatore Maugeri, Pavia, Italy, Chairperson of Women at Heart, and a member of the Board of the ESC, said: ‘The analysis of our Euro Heart Survey databases will be extremely interesting, as these are large databases on extensive European populations without the artificial representation so often seen in clinical trials. We have all the data at our fingertips and can reassess them in a relatively short time. These data are likely to give us important insights into manifestation, treatment and co-morbidity patterns, as well as hints on treatment and response trends, in women as compared with men. I am very much looking forward to the release of these data at our Stockholm Congress.’
What is already known is that women with heart disease are up to ten years older than men and present with much less obvious and stereotypical symptoms. They tend to have heart disease later than men due to the cardio-protective effects of oestrogen, which plays an important role up to the menopause. However, after the menopause, risks increase significantly and need delicate management.
In many women, the onset of heart disease is more gradual, accompanied by tiredness rather than the more commonly recognised symptoms predominant in men - e.g. sudden violent chest pain. Furthermore, women with CVD are more likely to die or suffer disability from a further attack or heart failure. Professor Priori said: ‘The issue is not simply that men and women are different per se, but rather that there are specific differences between the genders in symptom profiles and responses to treatment that must be taken into proper account.’
Physicians’ training is dominated by male data and trends, and guidelines focus on such data in recommending drug dosages and procedures. Thus women are being treated as if they are men, despite the notable differences in their disease elements.
• The ESC’s Women at Heart initiative is supported by an unconditional educational grant from the Bristol Myers Squibb Foundation.
• Information: www.escardio.org/initiatives/WomenHeart/
07.08.2006
More on the subject: