© BLU-MED Response Systems
Article • Healthcare facilities analysed
Cutting Coronavirus air contamination in hospitals
Preventing air contamination in healthcare facilities is crucial to minimise the airborne spread of Covid-19 and its new strains. Universal masking, rigorous use of and safe disposal of PPE, plus building ventilation are vital.
Report: Cynthia E. Keen
Twenty-four studies reporting hospital SARS-CoV-2 air contamination are summarised in a meta-analysis by a multi-institutional team of French researchers. These show that, although air around hospital in-patients with Covid-19 was frequently contaminated with SARS-CoV-2 RNA, it rarely was contaminated with viable viruses – with only very low concentrations of SARS-CoV-2 RNA in aerosols detected in isolation wards and areas where patients were on ventilation.
However, high concentrations of viral RNA were in public areas, e.g. hallways, public and staff restrooms, and medical staff dining and meeting rooms. Lead-author Gabriel Birgand PhD, at the Centre Hospitalo-Universitaire de Nantes, and co-authors, note that small areas are often poorly ventilated, and these rooms are where individuals tend to remove masks, even if only briefly.
Getting ventilation right

© BLU-MED Response Systems
Adequate building ventilation is crucial to contain disease. Negative pressure rooms – those with lower air pressure than their surroundings – are best for infected patients. When the door of a negative pressure room is opened, air in the room will not flow out. Non-contaminated filtered air will flow in, and exhaust systems, with filters that clean air before removal, prevent contamination outside the negative pressure rooms.
Additional to patient rooms, negative pressure rooms can include A&E waiting rooms, triage areas, and toilets. However, hospitals may not have such negative pressure in these areas and, with the surge of Covid-19 patients, not enough negative pressure patient rooms.
Rajesh K. Bhagat PhD and Professor Paul F. Linden PhD, at the University of Cambridge Department of Applied Mathematics and Theoretical Physics, recommend the use of either mechanical or natural displacement ventilation, where air intakes are at a low level and extracts are at a high level, as a viable alternative to negative pressure isolation rooms. Displacement ventilation produces negative pressure at floor and lower area of a room, drawing fresh air from outdoors, and positive pressure near the ceiling, compared to mixing ventilation, where air is circulated throughout the entire space of a room.
Recommended article

News • Comfy, but risky
Why many ventilation systems may increase risk of COVID-19 exposure
Ventilation systems in many modern office buildings, which are designed to keep temperatures comfortable and increase energy efficiency, may increase the risk of exposure to the coronavirus, particularly during the coming winter, according to new research.
Although, they explain, the concentration of contaminated air from Covid-19 patients in their hospital rooms is the same, with mixing ventilation flow, the contaminants are everywhere in the room in relatively low concentration, whereas with displacement ventilation, the contaminant is concentrated in a warm layer near the ceiling. Displacement ventilation relies on the fact that hot air generated by occupants or equipment rises and accumulates near the ceiling, where it can be rapidly and safely removed. Another advantage is that the ventilation rate required is much lower.
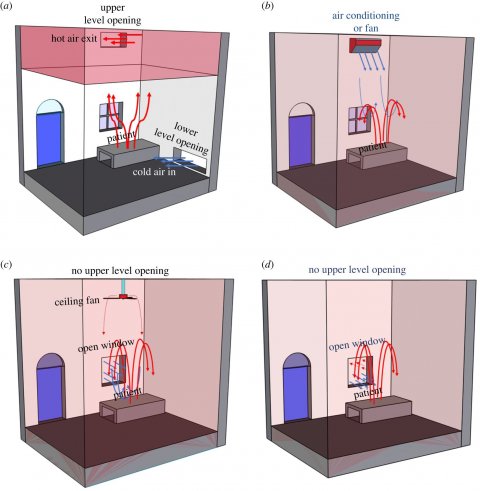
Image source: Bhagat et al., Royal Society Open Science 2020 (CC-BY 4.0)
The authors also recommend that extractor fans mounted near a ceiling could be installed to improve ventilation in existing facilities lacking openings for natural ventilation. In these, the air extraction flow rate, number of occupants in the room, and the unpolluted layer height need to be calculated.
Multinational authors of an online editorial in the International Journal of Environmental Research and Public Health recommend using evaporative humidifiers to maintain indoor relative humidity within the range of 40-60%. July 2020 research at the Leibniz Institute for Tropospheric Research (TROPOS), and the CISR National Physical Laboratory in New Delhi, suggests that transmission of coronavirus aerosol particles indoors seems to be strongly influenced by relative humidity. ‘If the relative humidity of indoor air is below 40%, the particles emitted by infected people absorb less water, remain lighter, fly further through the room, and are more likely to be inhaled by healthy people,’ explains lead author Ajit Ahlawat PhD, a research scientist in TROPOS’ Experimental Aerosol and Cloud Microphysics Department. ‘At a higher humidity, the droplets grow faster, fall to the ground earlier, and can be inhaled less by healthy people. Dry air also makes mucous membranes in our noses dry and more permeable to viruses.’
Experts’ recommendations
Along with using efficient portable air cleaners, limit the use of UV-C light to avoid ozone concentration indoors and, in hospitals and care homes, avoid aerosolised procedures using nebulisers during medical procedures. Instead, use a metered-dose inhaler for inhaled medications, to lower infection risk to medics. Also avoid spraying chemicals, such as hydrogen peroxide disinfectants.
Mobile testing units
Covid-19 mobile testing and vaccination units and field hospitals are functioning globally. The field hospitals come in 15- to 200-bed configurations and can be equipped with military specification rugged HVAC systems designed to operate in extreme hot or cold climates, using local power sources or freestanding generators operating at 50 Hz or 60 Hz. They can be equipped with negative pressure isolation systems that include isolation partitions, a negative pressure sensor and/or alarm, and optional restroom and shower facilities. ‘When BLU-MED medical facilities are used for isolating and treating patients with airborne or infectious diseases, we offer a negative pressure air scrubber equipped with HEPA and UV germicidal filtration,’ company president Donald A. Diesel PhD, told Healthcare in Europe. ‘This filtration unit attaches to the BLU-MED ECU and filters 100% of the return air, removing 99.984% of particulates 0.3 microns or greater in size.’
Source: YouTube/BLU-MED
In the above video he explains that each negative pressure isolation room consists of a floor, cover, end panel, and insulation liner. An alarm outside the room, monitoring an adjustable negative pressure range of 0.0254 to 0.1016 cm, enables nurses to monitor negative pressure. Inside the isolation area, air-conditioned air enters, circulates, and is removed, passing through both a HEPA filter and a germicidal filter at entry and exits. When not needed, negative pressure rooms can become positive pressure rooms.
18.02.2021