Sponsored • The Heraeus Symposium at DKOU
Challenges of periprosthetic infection
Periprosthetic joint infection (PJI) is on the increase internationally. In Germany, for example, around 14,500 cases of PJI in hip and knee replacements occur annually. 5,100 of those are caused by multidrug resistant pathogens.
Report: Beate Wagner
‘Eighty-seven percent of those affected die within five years,’ orthopaedic surgeon Professor Rudolf Ascherl MD pointed out during the Heraeus Symposium held at the German Congress of Orthopaedics and Traumatology (DKOU) held in Berlin, last October. Life expectancy is lower than for those affected by prostate cancer, breast cancer and melanoma, and quality of life is severely impaired. ‘The condition has chronic, almost oncological characteristics and patients suffer both physically and mentally for years,’ he added. ‘Twelve in 100 patients even state that they would rather die. We need a better understanding of who the high-risk patients actually are to get a better handle on PJI’, Ascherl believes.
The new classification may sound complicated, but it’s basically designed to clarify everything that needs to be addressed in a structured manner, before any kind of treatment
Volker Alt
According to British studies, overweight, multimorbid patients with heart, kidney or liver problems, and often further implants along with knee or hip endoprostheses, are at particular risk. ‘The present classification of PJI into acute or chronic stages does not sufficiently reflect the complex individual situation,’ according to Professor Volker Alt, from the Clinic and Polyclinic for Trauma Surgery at Regensburg University Hospital.
A new classification of PJI developed by Volker Alt and team now offers the prospect of improvement. This is to provide a clearer indication if a patient is still suitable for an intervention, from which type of intervention they could benefit and if, like many of those affected, they have already undergone one or several revisions. ‘Like other classification systems, PJI classification must consider all key factors, such as implant, pathogen and morbidities. The condition of the soft tissue, concomitant diseases and whether or not the patient can be anaesthetised are also important. The new classification may sound complicated,’ Alt observed, ‘but it’s basically designed to clarify everything that needs to be addressed in a structured manner, before any kind of treatment.’ ‘In future, all treatment options are to be based on this,’ Ascherl said.
PJI is one of the main reasons for around 72,000 revisions of hip and knee joint replacements. These often complex interventions carry a risk of their own. Amputation is not uncommon. ‘If patients wear unsuitable spacers for too long, for instance, or if foreign bodies are not completely removed, we should talk about the option of amputation,’ Ascherl explained. He recommends this in cases where sepsis and three relapses have already occurred. In each case, weighing up exarticulation and amputation must be on an individual basis.
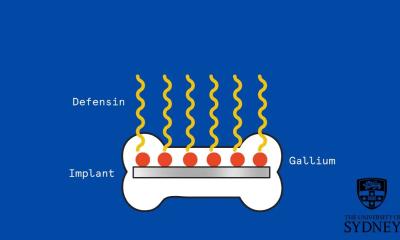
According to experts, the challenge of PJI can only be met in a multidisciplinary, professional setting – with a consistently standardised treatment algorithm, for instance – as implemented at the Centre for Musculoskeletal Surgery (CMSC) at the Charité University Hospital in Berlin. ‘Our multidisciplinary concept factors in specifics such as nosocomial pathogens, the condition of the bones and soft tissue, as well as the stability of the endoprosthesis,’ said Professor Andrej Trampuz, Specialist in Infectious Diseases and Head of the Department of Septic Surgery at the Charité Berlin. The standardised procedure has reduced the occurrence of relapses from 10.4% to 3.1%. ‘However, the increasing use of local antibiotics, implant coating and bacteriophages is new.’ Trampuz emphasised the importance of treating PJI as early as possible. ‘If the implant is to be preserved, the infection must not be older than a maximum of four weeks,’ the infection specialist advised. During this acute phase, sufficient surgical debridement, the administration of systemic and local antibiotics and, if applicable, the exchange of the mobile prosthetic components, have priority.
Once this early phase has passed, the persistent biofilms can no longer be eradicated even with biofilm-active antibiotics. ‘The objective is always the least invasive treatment option, with the best functional result without negative impact on the cure rate,’ Trampuz explained. ‘The importance of preserving the implant has increased considerably over recent years.’
After four weeks, PJI is regarded as chronic. There are around 6,500 of these late-stage infections every year, 4,000 in hip replacements and 2,500 in knee replacements. At this stage, those affected have now most definitely become high-risk patients. ‘If nosocomial pathogens are involved, when bones and soft tissue are in bad condition, and where the endoprosthesis is unstable, the only options are complete revision or lifelong suppression,’ said Trampuz.
Local, highly dosed administration prevents colonisation of spacers and supports the eradication of infection
Andrej Trampuz
The objective is always a one-stage exchange with a short interval. A Berlin study confirms the advantages. ‘Combined with local and systemic antibiotics this demonstrably reduces recurrences,’ he added. ‘During this late phase it’s important that the antibiotics are biofilm-active. Examples of this are rifampicin, ciprofloxacin, penicillin and fosfomycin. The combination of several antibiotics in the bone cement is advocated to prevent resistance. The different active agents attack the bacterial metabolism in different places. ‘My standard recommendation is the combination of clindamycin and gentamicin or a high dose of gentamicin plus vancomycin in the bone cement as they are locally effective, antibacterial and biofilm- active,’ Trampuz advised.
For primary joint replacements and aseptic revisions Trampuz recommends the prophylactic administration of 0.5-2g of antibiotic per 40g of cement; for septic revisions 2-4g per 40g cement. ‘Local, highly dosed administration prevents colonisation of spacers and supports the eradication of infection,’ he pointed out.
The combination of different antibiotics also produces important effects of synergy, as Professor Klaus-Dieter Kühn, from the Medical University of Graz reported. ‘Clindamycin for instance, is antibacterial in high concentrations, extremely able to permeate the bones and thus helps other antibiotics to move from cement into bone. There is also strong synergy between vancomycin and gentamicin. This combination has proved itself in the fight against multidrug resistant pathogens.’
Highly dosed, locally administered combinations of antibiotics are also suitable for infection prophylaxis. A British study involving 848 patients after bipolar hemiarthroplasty for displaced intracapsular femoral neck fracture showed that those who had been prophylactically given 1g each of gentamicin and clindamycin (Copal G+C) had a 66% significantly lower risk of infection than those with standard antibiotic loaded bone cement (0.5g gentamicin, Palacos R+G). Alt uses this protocol as standard at Regensburg University Hospital.
08.01.2020