Sponsored • Defibrillator or pacemaker?
Cardiac resynchronisation therapy improvements
Which CRT patients can be ‘downgraded’ from a CRT-D device with defibrillator function to a CRT-P with just a pacemaker function? This, with two further current CRT issues – chronotropic incompetence and telemonitoring of CRT patients – featured prominently at the Europace-Cardiostim Congress in Vienna.

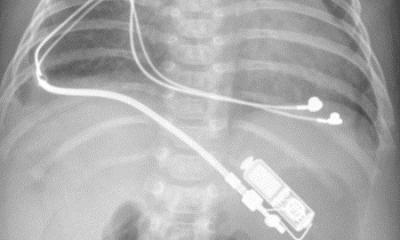
For more than 20 years, cardiac resynchronisation therapy (CRT) has been a pillar in the treatment of chronic heart failure (CHF). CRT devices are either pacemakers (CRT-Ps) or implantable defibrillators (CRT-Ds), which are implanted in the patient’s chest. These are connected to the heart with three leads, the third one linking to the left ventricle which pumps blood through the body. While both types of devices synchronise the heartbeat, CRT-Ps prevent the heart from beating too slowly and CRT-Ds prevent it from beating too quickly.
At a satellite symposium at the Europace-Cardiostim Congress (EHRA 2017) experts debated whether patients who respond well to a CRT-D and show improved heart function should receive a CRT-P in the next scheduled device replacement. The background: Many patients respond so well to CRT that their heart function markedly improves and a CRT-D might not be needed; indeed between 10-25% are so-called super-responders, i.e. their cardiac device restores a normal ejection fraction in the left ventricle, lowering the risk of sudden cardiac arrest to that of a healthy person.

At EHRA 2017, Dr. Jacques Mansourati from Brest University Hospital in France, presented a study investigating this very issue: The BioContinue study is observing 277 CRT patients in eight countries to determine which patients need a defibrillator. According to preliminary study data, 39% of patients who receive a CRT replacement do not need a defibrillator because the therapy increased the ejection fraction of the left ventricle by at least 40% and no ventricular tachycardia was reported. ‘During a scheduled replacement of the device, responders and super-responders can be downgraded from a CRT device with defibrillator to one without this function,’ Mansourati explained.
The second controversial issue in CRT is chronotropic incompetence: In 20-40% of all CRT patients, heart rate does not increase commensurate with increased physical activity. ‘Chronotropic incompetence could be a major factor in patients who do not respond to CRT,’ said Dr. Mattias Roser from Charité Berlin. In these cases, Roser points out, rate-adaptive pacing might provide a solution, as indicated by BioCreate, a pilot study conducted at Charité to investigate whether Closed Loop Stimulation in heart failure patients with chronotropic incompetence can improve clinical outcomes. This technology, developed by Biotronik, responds naturally to patients’ physical and mental activity or stress, adapting heart rates physiologically. Roser is optimistic: ‘We consider this a highly potential approach to significantly improve the treatment of CRT patients,’ he said.
The third, but by no means least, important issue is remote monitoring of ICD patients. Ever since the IN-TIME study showed Biotronik Home Monitoring reduced mortality in heart failure patients, the use of this technology has been included in the clinical guidelines. However, data presented at EHRA 2017 indicate that not all tele-monitoring systems are created equal: they do offer different clinical outcomes. TRUECOIN, a meta-analysis, showed Biotronik Home Monitoring to reduce mortality in all types of ICD patients.
Source: Biotronik
28.08.2017