© goanovi – stock.adobe.com
News • Kinetic analysis of therapeutics
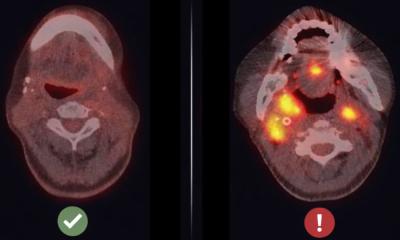
How boron may point the way to better therapies for head and neck cancer
Real-time measurement of boron in live cells explains how drugs travel in and out of tumour cells
A new technique has measured boron in individual cancer cells for the first time, enabling researchers to better understand how drugs act to kill tumours in some cancers.
In a new article in the Journal of Analytical Atomic Spectrometry, a team from the University of Birmingham funded by the Rosetrees Trust have for the first time used a technology to conduct real-time measurement of boron in live tumour cells. The technique, called single-cell inductively coupled plasma mass spectrometry (ICP-MS), enabled the team to see how and when treatments for head and neck cancers enter and exit tumour cells.
We now have the first direct evidence of how much boron is present in individual tumour cells, and how long it stays there. This information could help to optimise when neutron irradiation should be delivered relative to drug administration
James Coverdale
Boron Neutron Capture Therapy (BNCT) is a new form of therapeutic for head and neck cancer that involves patients taking a drug containing the element boron that accumulates in tumour cells. The tumour is subsequently irradiated with neutrons that interact with boron which selectively kills cancer cells. BNCT relies on the drug getting into cancer cells at a sufficient level and then remaining there long enough for the neutron irradiation to be administered. With this newly tested technique, researchers can begin to understand how to most effectively deliver BNCT for patients with head and neck cancers as a precision treatment.
Dr James Coverdale from the School of Pharmacy at the University of Birmingham said: “Until now, it’s only been possible to measure average boron uptake in hundreds-of-thousands of cells, which masks important differences between individual cells. Our single-cell approach reveals this variability, which is critical in a tumour setting where heterogeneity often determines whether treatment works or fails. We believe the results are exciting because we now have the first direct evidence of how much boron is present in individual tumour cells, and how long it stays there. This information could help to optimise when neutron irradiation should be delivered relative to drug administration. By showing which transport pathways bring boron into cells, the work also offers clues for designing better drugs that accumulate more effectively. For the cancer drug discovery community, this study opens a new way of evaluating BNCT drug candidates.”
A key breakthrough was creating the right environment for cells to stay alive long enough for measurement, while maintaining compatibility with the highly sensitive equipment. This challenge required the team to carefully optimise both the culture medium and the way cancer cells were introduced into the instrument. Without this step, the cells would rapidly deteriorate, making it impossible to capture meaningful data.
Jack Finch, co-first author of the study and University of Birmingham Biochemistry alumni said: "This will be vital for testing and comparing future BNCT drugs and will help to identify the most effective treatments. Ultimately, our work supports progress toward making the already promising BNCT into a more precise and effective cancer treatment."
According to Cancer Research UK, Head and neck cancer is the 8th most common cancer in the UK, accounting for 3% of all new cancer cases (2017-2019).
Source: University of Birmingham
12.09.2025