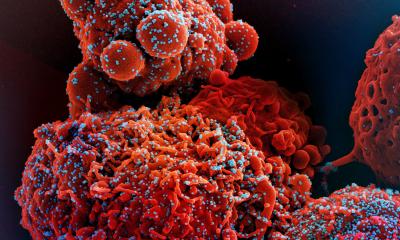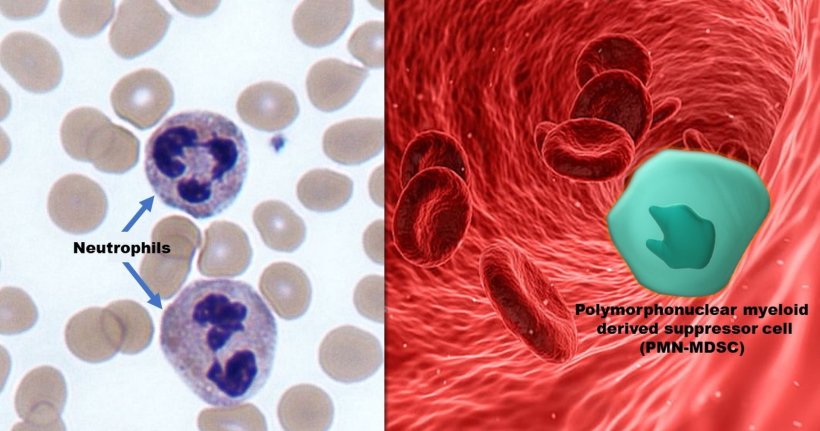
Image credit: Photomicrograph of neutrophils (left side) courtesy of Dr. Graham Beards via Wikimedia Commons and PMN-MDSC graphic (right side) created by M.E. Newman, Johns Hopkins Medicine, using public domain images
News • From neutrophil to PMN-MDSC
Blood cell corruption identified as path to severe Covid
A federally funded Johns Hopkins team finds the virus ‘reprograms’ neutrophils to impair production of immune cells critical for fighting Covid
A National Institutes of Health (NIH)-funded study by researchers from Johns Hopkins Medicine, the Johns Hopkins Bloomberg School of Public Health and The Johns Hopkins University Whiting School of Engineering finds that neutrophils — the most abundant type of white blood cells in humans — may be altered by Sars-CoV-2, the virus that causes Covid-19, to cease their normal function of destroying pathogens in the body and, instead, significantly inhibit other immune cells critical for fighting the virus.
The study was posted in the journal Science Translational Medicine.
“Our findings suggest that in some Covid infections, Sars-CoV-2 may dramatically impair the immune response by reprogramming neutrophils — front-line immune cells central to fighting infections — into a cell type called polymorphonuclear myeloid derived suppressor cells, or PMN-MDSCs,” says study senior author Andrea Cox, M.D., Ph.D., professor of medicine and oncology at the Johns Hopkins University School of Medicine. “PMN-MDSCs are known to suppress virus-fighting immune cells known as T lymphocytes, or T cells, and we believe the reprogramming that creates them could provide a mechanism by which severe Covid, a more dangerous form of the disease, may arise.”
Recommended article
Article • Covid-19
Coronavirus update
Years after the first outbreak and spread of coronavirus Sars-CoV-2, its impact can still be felt in everyday life. Keep up-to-date with the latest research news, political developments, and background information on Covid-19.
According to the U.S. Centers for Disease Control and Prevention (CDC), severe Covid cases are those that result in hospitalization, admission to the intensive care unit, intubation or mechanical ventilation, or death. The CDC estimates that approximately one in six Americans who get Covid-19 will experience serious complications, with the highest risk among people 65 or older, and those who are immunocompromised. “Previous research has shown that severe Covid-19 is associated with an increased number of neutrophils in the blood,” says study lead author Leon Hsieh, Ph.D., who worked on the research team as a student in Cox’s lab and now is a postdoctoral fellow at NYU Langone Health. “Our goal was to find out whether these neutrophils had been reprogrammed by Sars-CoV-2, and if so, did they contribute to the shift from mild infection to a more serious form of Covid-19.”
PD-L1 antibodies may provide a means of treating people with severe Covid in combination with antiviral medications or as a stand-alone therapy when a patient is unable to take antiviral medications
Andrea Cox
In their study, the researchers examined neutrophils found in blood samples from 39 participants hospitalized in the Johns Hopkins Health System in 2020 for acute Covid-19 that became severe, and from nine people without a Sars-CoV-2 infection (as healthy controls for comparison). All of the participants were unvaccinated against Covid-19 as their blood was collected before immunizations were available. Participants with Covid-19 who had been given dexamethasone or other corticosteroids that suppress the immune system were not included in the study.
“What we found upon examining the neutrophils is that in people with Covid-19, the cells had degranulated [released their granular contents into the surrounding environment] and differentiated into PMN-MDSCs, which are known to suppress T cells — and therefore, the immune system — in cancers and other non-viral diseases,” says Cox. “We believe that this may be the first time PMN-MDSCs have been seen in a respiratory viral infection, so we had a golden opportunity to explore any role that these cells might have with the development of severe Covid-19.”
PMN-MDSCs associated with cancers and other nonviral diseases, Hsieh says, are known to have two key proteins on their surfaces that negatively affect the immune system: lectin-type oxidized low-density lipoprotein receptor-1 (LOX-1) and programmed cell death ligand 1 (PD-L1). While the role of LOX-1 on neutrophils remains unclear, PD-L1 is well known for binding to a specific receptor, called PD-1, on T cells, which inhibits their activation, proliferation, differentiation and ability to signal other immune cells to the presence of a pathogen. “When we compared neutrophils from people with severe Covid to those with mild to moderate Covid, we found that the cells from the former were more likely to express LOX-1 and PD-L1,” Hsieh says. “Taking it one step further, we cultured neutrophils in the presence of SARS-CoV-2 in the lab, which induced the neutrophils to differentiate into PMN-MSDCs that were capable of limiting T-cell proliferation and inhibiting T cells from releasing cytokines, the signaling proteins that help rally the immune system against a pathogen threat.”
Hsieh says the researchers also co-cultured neutrophils with H1N1 influenza virus, but did not see any conversion to PMN-MDSCs. Additionally, an earlier study reported that PMN-MDSCs were not found in people hospitalized with severe influenza infections. “So, it appears that not all viruses can cause the differentiation.”
Cox says the team’s findings suggest that Sars-CoV-2 may directly induce neutrophils to take on the functions of a PMN-MDSC, and in turn, weaken the immune response against the virus enough to cause severe Covid. Better understanding the mechanism for neutrophil conversion into PMN-MDSCs may lead to new therapy options for severe Covid. In fact, she explains, a potential treatment might already exist. “Antibodies against PD-L1 have been used to treat cancers, so we tried adding them in the lab to neutrophils co-cultured with Sars-CoV-2 and then looked at how this affected a converted neutrophil’s ability to weaken the immune system,” she says. “T-cell suppression was reduced, and T-cell activity — marked by the release of cytokines — increased; therefore, PD-L1 antibodies may provide a means of treating people with severe Covid in combination with antiviral medications or as a stand-alone therapy when a patient is unable to take antiviral medications.”
Along with Cox and Hsieh, the members of the research team from Johns Hopkins Medicine and the Johns Hopkins Bloomberg School of Public Health are Tihitina Aytentisu, Franco D’Alessio, Emily Egbert, Alexia Figueroa, Naina Gour, Nirvani Jairam, Andrew Karaba, Petros Karakousis, Aaron Milstone, Alvaro Ordonez, Andrew Pekosz, Katerina Roznik, Eileen Scully, Elizabeth Thompson and Weiqiang Zhou.
Source: Johns Hopkins Medicine
23.05.2025