Article • Cardiology
Big data in cardiac CT
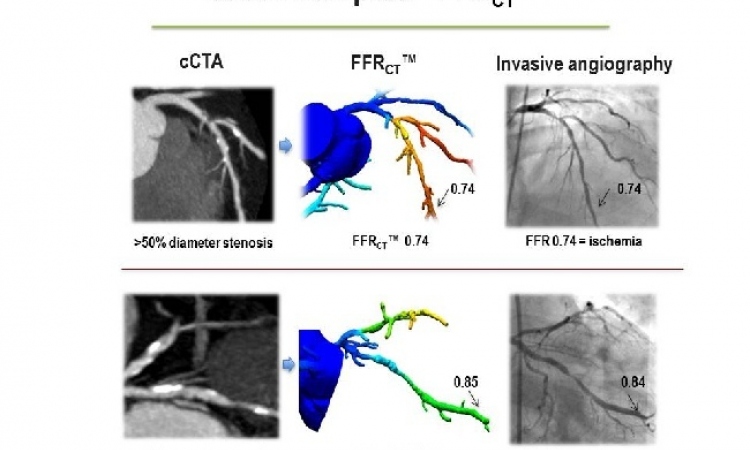
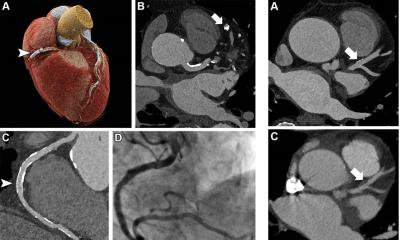
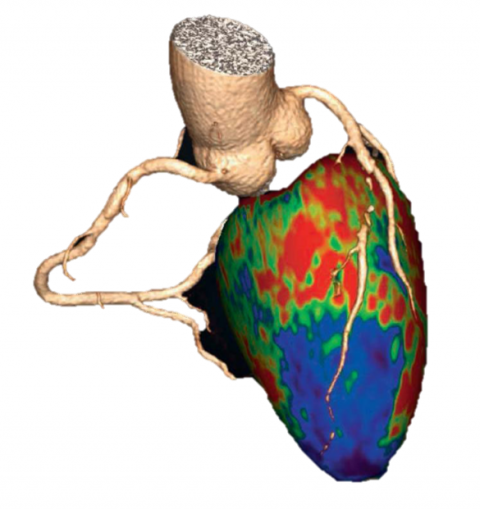
CT angiography (CTA) is evolving from a morphological – anatomical – to a functional imaging modality. In the past two years, cardiac CT perfusion measurement techniques were launched that predict which lesion will cause a reduction in blood flow.
Report: Michael Krassnitzer
‘We are getting closer to our objective: to be able to predict, by non-invasive means, the consequences of a stenosis in a individual coronary heart disease patient and to evaluate whether and which intervention will be useful,’ says Uwe Joseph Schöpf MD, professor of radiology, cardiology and paediatrics and Director of Cardiovascular Imaging at the Medical University of South Carolina in Charleston, SC, adding: ‘This is bona fide personalised medicine.’
Today, tube voltage and tube current are automatically adapted to each individual patient during a cardiac CT scan. Moreover, the new generation of multi-detector CT systems offer new insights: dual energy scanners, i.e. scanners that use two tubes in one scan, enable assessment of blood content in the heart muscle. ‘We can directly and dynamically measure blood flow within the heart by scanning quickly back and forth across it while the contrast agent bolus moves through the heart muscle,’ Professor Schöpf explains.
Another promising technology is the single photon detector, currently under development. ‘These detectors allow us to look at each individual photon and its behaviour which provides new data for tissue characterisation, for example the distribution of iodine in the body,’ he adds.

The development of new algorithms and statistical procedures is contributing to the rapid progress in imaging technologies. Thermodynamic models are being used to predict blood flow, or even more impressive, artificial intelligence concepts are applied in radiology. Computers ‘learn’ by analysing hundreds of cases of coronary stenoses to determine which stenosis will be dangerous for the patient. Schöpf sees enormous potential: ‘This is a Big Data application, but by no means science fiction. Initial results are expected to be published later this year.’
The new techniques and procedures have an important positive side effect: radiation dose will be drastically reduced again. Today, a full CTA can be performed at 80 kV with 30 ml contrast. A study at the Medical University of South Carolina, co-authored by Professor Schöpf (Spearman et al, Radiology, 16 Oct 2015) indicates that the introduction of automated kV selection in 80,000 exams, worldwide, reduced average radiation dose by 14 percent – a result which, a few years ago would have been considered revolutionary. Albeit, as Professor Schöpf points out, ‘Here, in the US, the discussion about radiation dose is petering out.
Radiation dose as a dominant issue, above all in the USA, appears to have been largely a matter of domestic political interests. Many radiologists assume that radiation dose was used to prepare the ground for ‘ObamaCare’: an argument to decrease the use of imaging in order to save as much money as possible in the context of the planned US healthcare reform.’
Today, with President Barack Obama’s healthcare reform being well established ‘the issue of radiation dose has all but disappeared,’ Schöpf observed.

However, on the level of technology dose reduction remains important, the professor emphasises. The objective is to further reduce radiation and contrast dose while achieving the same high level of image quality. According to Schöpf, results so far are encouraging and, in some cases, image quality was even enhanced. ‘What we need to do now,’ he believes, ‘is to enhance our diagnostic expertise.’
Tissue characterisation, dual energy, single photon detectors – these are the current top priorities on the research agenda.
However, for Schöpf there are even more important questions to be answered: ‘We know that CTA is a good, precise and patient-friendly procedure. Now we need to ask how we can make best possible use of this procedure. Is it cost-efficient? Which clinical scenarios can we envisage? Which patient cohorts will benefit most from these new procedures? Where should these exams be performed? These are crucial issues we must deal with in the coming years.’ While clinical evidence does exist, as Schöpf points out, ‘Our focus is on the creation of even more evidence that tells us where CTA should be applied.’
Profile:
Austrian-born Uwe Joseph (Joe) Schöpf is a professor with appointments in Radiology, Cardiovascular Medicine and Paediatrics at the Medical University of South Carolina (MUSC) in Charleston, SC. There he directs the Cardiovascular Imaging Division and is Director of Computed Tomography Research and a Director of the University Designated Centre for Biomedical Imaging. Schöpf grew up in Munich, Germany, where he graduated in medicine at Ludwig Maximilian University (LMU) and received specialist training at its Institute of Clinical Radiology. In 2001, already an accomplished radiologist, he left Munich to pursue his interest in cardiothoracic imaging at Brigham and Women’s Hospital, Harvard Medical School, in Boston, MA. The professor joined MUSC in 2004.
ECR 2016 - Don't miss
Wednesday 2 March, 10:30–12:00 Room M 3
The evolving role of cardiac CT
01.03.2016