Fame 2 rates FFR as a new gold standard
John Brosky reports on a ground-breaking trial and how CT-FFR may change the practice of invasive cardiology and cardiac surgery.
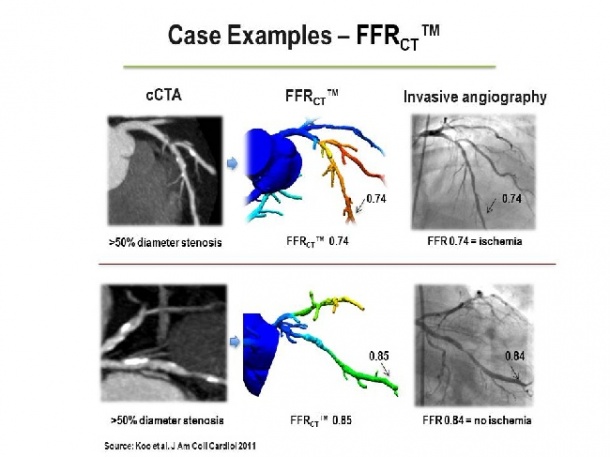
Note the close correspondence between FFRcT™ and invasively-measured FFR. Non-invasive FFRcT™ is computed from conventional cardiac cT angiography images and can be determined throughout the coronary tree.
Images by courtesy of heartflow, U.S.A.
Note the close correspondence between FFRcT™ and invasively-measured FFR. Non-invasive FFRcT™ is computed from conventional cardiac cT angiography images and can be determined throughout the coronary tree.
Images by courtesy of heartflow, U.S.A.
Watching the grey angiography images of a beating heart, it is often clear where arteries are pinched or blocked. The temptation is to re-open each lesion with angioplasty and then place a stent to be sure the artery stays open. This seemingly safe-sounding approach turns out to be excessive, leading to unnecessary stenting. First, cost to the healthcare system for the procedure is high. Then there is risk for patients, as cardiologists agree implanting a stent to fix coronary artery disease is equivalent to implanting a new disease with the risk of in-stent thrombosis. Now, however, thanks to a technique called fractional flow reserve (FFR), each artery can be evaluated to determine which of the pinch points is actually the ‘culprit lesion’ causing the patient’s distress. Using a pressuresensitive tip on a guide wire, the cardiologist can measure blood flow on either side of the lesion. In January 2009 the New England Journal of Medicine published results from the clinical trial, Fractional Flow Reserve versus Angiography for Guiding PCI in Patients with Multivessel Coronary Artery Disease (FAME), showing that the FFR measure significantly improves clinical outcomes. Put into practice, FFR also reduced the excessive stenting of patients.
The follow up clinical trial FAME 2, which compared use of FFR against managing patients with medications, proved to be so good that it had to be stopped. Enrolment in the trial was halted as the independent data safety monitoring board concluded it was unethical to randomise patients away from the arm of the study offering fractional flow reserve (FFR). The board found a highly statistically significant reduction in the need for unplanned hospital readmission and urgent revascularisation when FFR-guided assessment was used to direct treatment in patients with coronary artery disease. David Holmes MD, the recent president of the American College of Cardiology (ACC), commented, ‘FAME 2 tells us to treat ischaemia and not lesions. It is a ground-breaking trial that changes clinical practice.’ Endorsed with the highest recommendation in the European Society of Cardiology guidelines, FFR is now the gold standard for a clinical decision to treat coronary lesions with stents.
Drug-Free FFR
Although the high profile success of FAME has greatly boosted sales of FFR systems, despite its effectiveness FFR is not widely used. In the USA, for example, its use is estimated to be less than 10% of stenting decision-making. A key reason is that as a patient is at rest during the procedure, the physician needs to inject the pharmaceutical stress-maker adenosine to simulate heart function and simulate chemically the pressure levels detected by FFR. The drug is contra-indicated for a significant number of conditions and, for acute patients, the ones where a decision on multiple stenting needs to be made quickly. In November 2011, a team from Imperial College, led by Justin Davies MD and Sayan Sen MD, presented an alternative technique for measuring the severity of a coronary stenosis, which is similar to FFR. Called Instant Wave-Free Ratio (iFR) it does not require a pharmaceutical boost for a pressure-derived index scoring system. The multi-centre ADVISE study assessed 157 stenoses in 131 patients, demonstrating an overall diagnostic accuracy of 88%.
In May 2012, at EuroPCR in Paris, Dr Davies presented a registry of 339 patients from the ADVISE study where he claimed a 94% diagnostic accuracy for the new technique, iFR. He concluded that adenosine does not add any incremental benefit to the diagnosis. He said that iFR is easier to use, can be indicated for far more patients, and makes the procedure faster. ‘The work on FFR has been fantastic,’ he said. ‘But today we are in a different era with computational power that did not exist when the FFR calculations were developed.’
Making a quantum leap in processing power to the level of a super-computer brings a new method of ‘virtual FFR’ for measuring the severity of coronary lesions Software developed by a team from Stanford University (Palo Alto, California) has demonstrated that a haemodynamic modelling of the heart created on a supercomputer using digital data from a common CT scan can accurately identify vulnerable plaque formations.
Virtual FFR with any CT
The virtual CT-FFR technique being brought to market by the start-up firm HeartFlow (Redwood City, California) presents a non-invasive, desktop alternative with a point-and-click capability to read FFR for a specific patient in any coronary artery on a 3-D map of the heart, rather than one-by-one while the patient is lying on the cath lab table. HeartFlow won the Innovation Award from the Board of EuroPCR in 2011, which found CT-FFR to be ‘potentially disruptive to the diagnosis and treatment of patients with stable ischaemic heart disease . . . [and] it may change the practice of invasive cardiology and cardiac surgery.’
To obtain a virtual FFR exam, a radiologist uploads a 20 megabytes file with the raw DICOM data from any CT coronary exam. There is no need to run an additional exam, any recent data set will do. Five hours later the radiologist receives from HeartFlow a 3-D dynamic flow map of the patient’s heart generated by the super computer. According to HeartFlow CEO John Stevens, 40 million coronary diagnostic tests are ordered annually worldwide, 24 million in the USA alone. The cost for the service ‘will be vastly less expensive than going to a cath lab and measuring FFR,’ he said. Yet, the target for virtual FFR is not necessarily FFR. He pointed out that a pre-operative CT-FFR assessment might prove an alternative to other non-invasive tests for assessing coronary artery disease -- such as stress echo or nuclear medicine. ‘Stress echo, SPECT and CTA,’ he said, ‘are suboptimal examinations compared to FFR, which has proven to be so precise and today is so valued as a tool. ‘We need to do a lot better with the number of coronary studies and the accuracy of these exams.
25.08.2012





